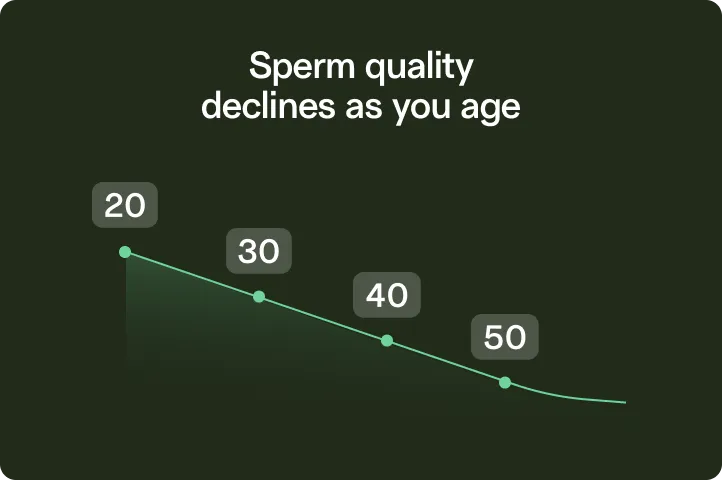
Fertility declines with each birthday
Past 35, you’re more likely to deal with infertility — and your child has a higher risk of conditions like autism.
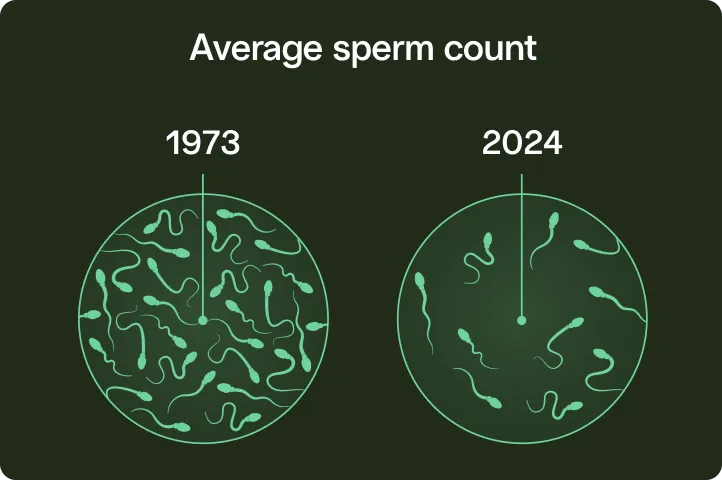
Our sperm is not okay
Sperm counts have dropped over 50% since the 1970s, thanks to chemicals, plastics, and our modern lifestyles.
Clinics are awkward and expensive
With the old-school approach, you wait months for an appointment in the communal “collection room” (yikes).


We’ve supported over 30,000 future parents
Trusted by top fertility experts, the US military, and people like you.

I was in a time crunch because my husband was having surgery. They were so courteous. Assisted me through the whole process. So grateful for all the help, patience and understanding.
Angeline Davis
Verified client
It was super simple and my insurance covered it.
Austin
TRT Patient

2024
Best Option for Sperm Testing & Freezing
Legacy is a game changer in the male fertility space.
4.9
130+ Google Business reviews

Mail-in kits can be a simple way to screen for any underlying sperm problem. This is a great option if you are not comfortable taking a specimen to the lab.
Stanton Honig, MD, Professor of Clinical Urology













