Transgender Woman Fertility Preservation
For those whose gender identity doesn’t align with their biological sex, proactive fertility preservation is especially important for family-building. Gender-affirming hormone therapy and other aspects of gender transition can have a significant impact on a person’s fertility and ability to produce healthy sperm. Proactive fertility testing and sperm freezing can help with fertility preservation and create a pregnancy later in life.
Read on to understand more about fertility preservation and sperm freezing for trans women, and how Legacy’s at-home sperm freezing kits and semen analysis can help.
While we’ll be using the phrases “trans women” and “transgender women” here, this guide applies to any sperm-producing person considering gender transition, regardless of identity.
Photos courtesy of The Gender Spectrum Collection.

Table of contents:
- Gender transition: an overview
- How male-to-female gender transition affects fertility
- Tucking and sperm health
- Gender-affirming hormone therapy and fertility
- Fertility after bottom surgery for trans women
- Sperm freezing (sperm cryopreservation) for trans women
- When should a trans woman freeze her sperm?
- Sperm freezing costs for trans women
- Family building for transgender women
- Fertility resources for trans women
- References
Gender transition
There are three possible “steps” in gender transition. Which steps a person undertakes, and the timeline between them, is individual, and dependent on their personal gender identity, how they want to present, their financial resources, and their medical history. Understanding these steps is crucial to deciding when to pursue fertility preservation.
Social gender transition
During this step, a person may change their pronouns and/or name. They may “come out” as trans to their family and friends. They may also change their appearance and clothing. Often, the goal is to affirm a person’s gender identity by adopting a more feminine or gender-fluid presentation.
Medical gender transition
At this step, a person may seek care from a medical provider to access gender-affirming hormone therapy. For assigned-male-at-birth people, this hormone therapy usually involves taking estrogen, often considered a “female” hormone (although all sexes produce some level of estrogen).
Many trans women also take anti-androgen medications. Androgens, such as testosterone, are “male” hormones that are found in higher levels in sperm-producing people; anti-androgens or “androgen blockers” are medications that prevent testosterone from affecting the body as it typically would.
Hormones like estrogen and testosterone affect secondary sex characteristics. Taking estrogen, and blocking the effect of testosterone in the body, allows a trans woman to develop more typically feminine features, such as breasts, wider hips, smaller arms, and finer, slower-growing facial and body hair.
As gender-affirming hormone therapy can have a significant impact on a person’s ability to produce healthy sperm, fertility preservation, namely sperm freezing options, can be considered at this stage.
Surgical gender transition
There are many different directions a trans woman can take with surgical transition. “Top surgery” refers to surgery performed above the waist; for trans women, that’s sometimes breast augmentation (implants). “Bottom surgery” is surgery performed below the waist, typically to the genitals.
Bottom surgery may involve one or more of these three options:
- Orchiectomy. An orchiectomy is the removal of the testicles from the scrotum. Because the testicles produce testosterone, removing them may make gender-affirming hormone therapy simpler, allowing a transfeminine person to stop taking anti-androgens and take lower levels of estrogen.
- Vulvoplasty. During vulvoplasty, a surgeon uses the tissue from the penis and scrotum to create a clitoris, urethra, and labia. After vulvoplasty, a trans woman will not have a vaginal canal, but will have the outward appearance of female genitals.
- Vaginoplasty. This surgery is similar to vulvoplasty, except that in addition to the clitoris, urethra, and labia, the surgeon will create an internal vaginal canal between the rectum and the bladder.
These surgeries involve different levels of complexity and recovery. Not every trans woman will choose to have bottom surgery (or surgery at all).
Male-to-female gender transition and fertility
The process of gender transition may affect fertility in several different ways. Learning the potential effects is important when considering fertility preservation.
The impact of “tucking” on sperm
Some trans women who are pre-operative or have not chosen surgery practice tucking, a way to hide the penis and the testes. Tucking can be done by moving the penis and scrotum between the buttocks, or by pushing the testicles up into the inguinal canals (where the testicles reside before “dropping” during infancy), and securing with tight underwear or tape.
While tucking gives a more desirable presentation for many trans women, it can be damaging to spermatogenesis, the process of sperm production in the testicles. Testicles hang away from the body in the scrotum because sperm production requires a temperature approximately 5.5ºF lower than body temperature. Tucking or wearing tight undergarments increases the heat in the scrotum by up to 5ºF, impairing sperm production. This may be why trans women are more likely to have have poor sperm quality compared to cis men, even before they begin hormone treatment.
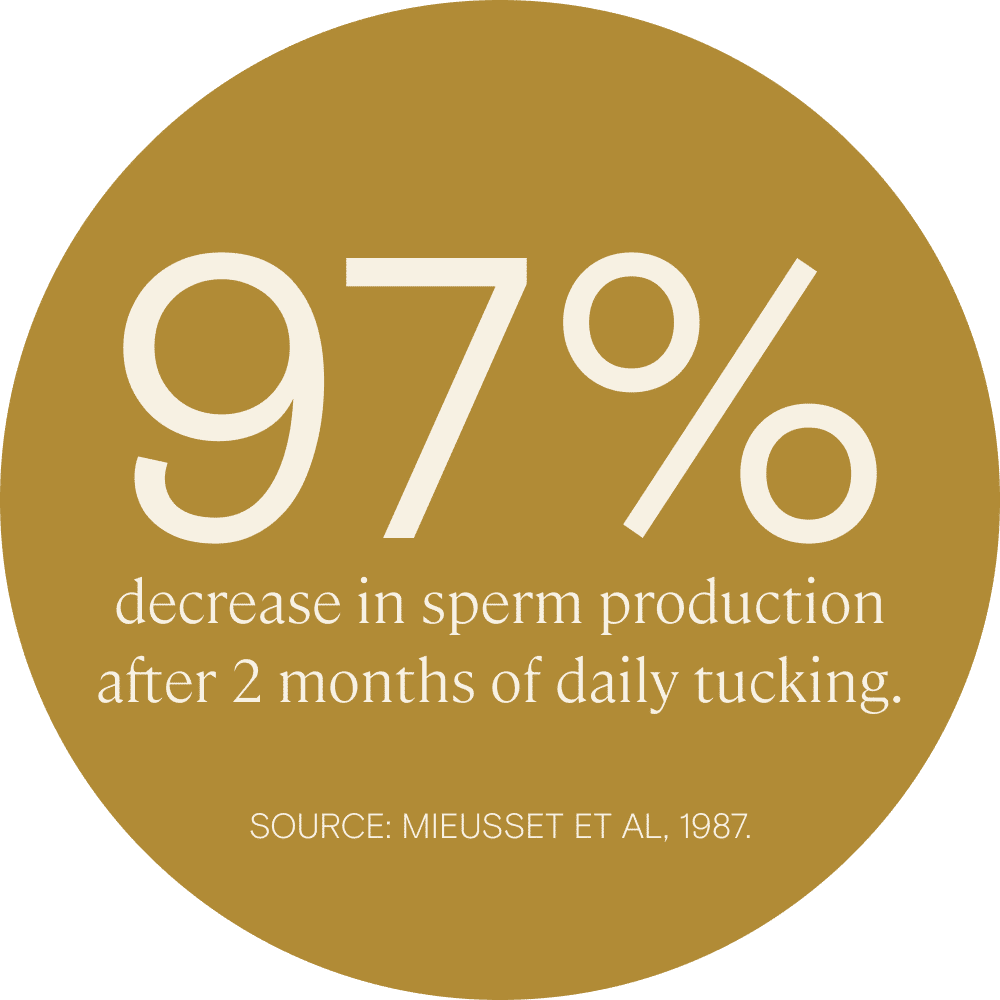
The correlation between tucking and low motile sperm count has been directly demonstrated. In fact, the act of tucking has been investigated as a potential contraceptive practice for cis men in several studies. In one study, researchers found that those who practiced tucking had very low motile sperm counts and a 0% pregnancy rate. In another, sperm production decreased by 97% after 2 months of daily tucking.
The good news is that sperm impairment caused by tucking appears to be entirely reversible within several months of pausing the practice. Still, this may be an important consideration for trans women who are considering sperm freezing for potential use later.
Gender-affirming hormone therapy’s effect on fertility
Testosterone is essential to the production of sperm. It plays a role in initiating several key processes in spermatogenesis, including the division and maturation of sperm cells. The goal of hormone therapy for transgender women is to decrease testosterone and increase estrogen levels to create a more typically feminine appearance. Estrogen therapy helps decrease testosterone levels in the body. Many trans women also use anti-androgens to further decrease their testosterone to typical female levels (around 70 ng/ml).
Testosterone levels under 264 ng/ml are associated with poorer semen parameters. And, as we would expect, use of estrogen and androgen-blockers is associated in research with poor sperm quality and lower sperm count. A 2017 review looked at nearly 40 years of research on the impact of cross-sex hormones on the sperm quality and testicular function of trans women. The review found that, in the majority of cases, estrogen and/or anti-androgen treatment caused reduced or halted spermatogenesis, as well as physical changes to the testicles.
How long does it take for hormone replacement therapy (HRT) to impair fertility?
The effect seems to be dose-dependent. In one study, a low-dose estrogen therapy had no impact on sperm concentration or motility, while a higher-dose regimen resulted in reduced sperm motility after just a few days and reduced sperm concentration after 2 weeks. Fertility preservation, including proactive sperm freezing, can help mitigate this.
Is infertility caused by gender-affirming hormones reversible?
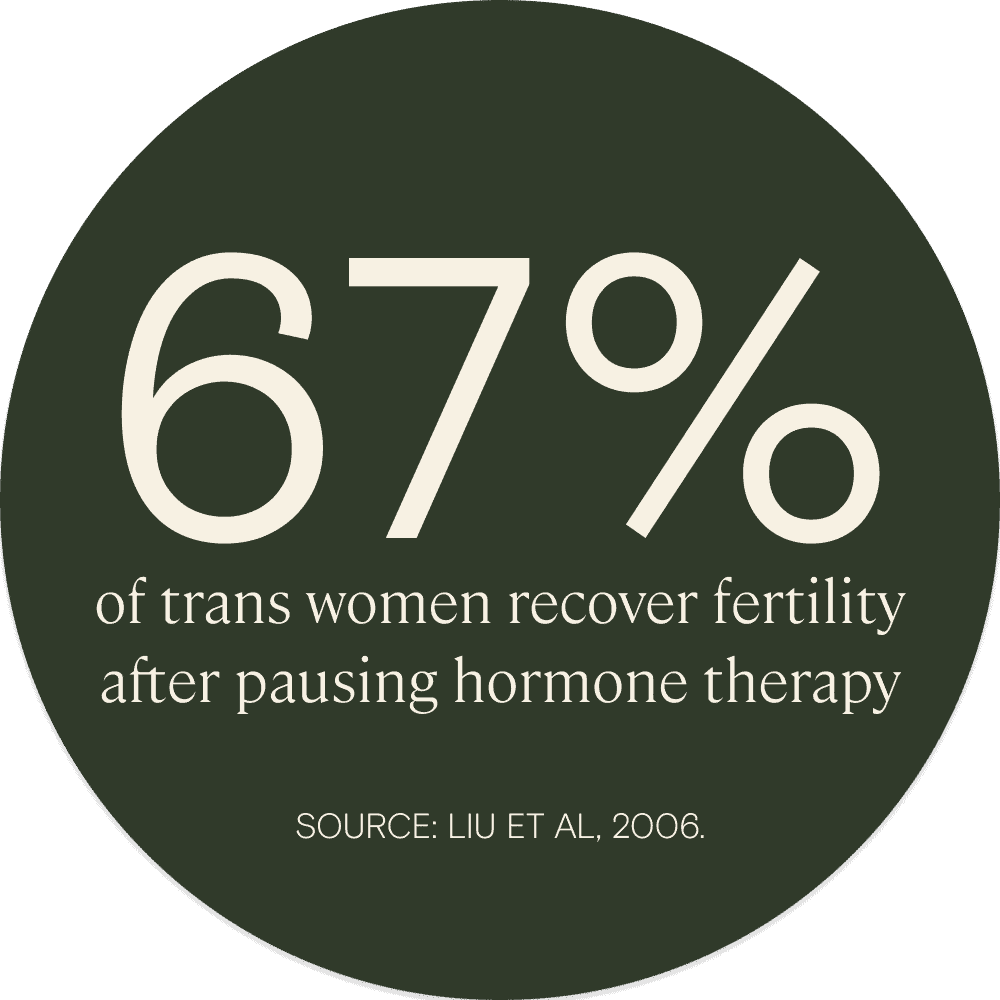
In some cases, it appears to be. One study suggested that, within 6 months of stopping estrogen therapy, 67% of subjects recovered a normal sperm count.
However, the impact of medical gender transition on fertility, as well as the capacity for spermatogenesis to recover if estrogen treatment is paused, seem to be variable and individual. Case studies demonstrate that, while some patients continued spermatogenesis through gender-affirming hormone treatment, others stopped producing sperm altogether, and several experienced azoospermia for 4–5 months after pausing therapy.
The fertility impact of bottom surgery for trans women
Sperm is produced in the testicles, and gender-affirming bottom surgery for trans women involves the removal of the testicles. Therefore, while most people who opt for bottom surgery retain sexual function, it’s not possible to recover sperm production or “natural” fertility after bottom surgery. That’s why many trans women consider sperm freezing options before surgical transition or have a testicular sperm extraction (TESE) at the time of bottom surgery.
Learn more about fertility preservation, sperm freezing and our at-home sperm freezing kits in our Guide to Sperm Freezing.
Sperm freezing for trans women
The primary fertility preservation option for assigned-male-at-birth trans people is sperm freezing or cryopreservation. Sperm freezing is the process of freezing one or more semen “samples,” or ejaculations, for potential use to attempt to conceive later on.
The process of sperm freezing is as follows: A person will produce a semen sample via masturbation. That sample is then brought into a lab, processed, and analyzed to determine that it’s healthy enough for sperm freezing. If it is, it’s plunged into liquid nitrogen to quickly bring it to a temperature of -196ºC, at which point all biological processes stop. Then it can stay cryogenically stored indefinitely.
Learn more about sperm freezing and sperm freezing costs with Legacy’s at-home sperm freezing kits.

Legacy’s at-home sperm freezing
In the past, the process of sperm freezing required you to visit a fertility clinic or sperm bank to produce a semen sample in a “collection room” on-site. This can be an uncomfortable experience for many people, including trans women. Legacy offers at-home sperm freezing kits and semen analysis that allows you to mail your sample to our labs for clinic-grade analysis and cryogenic storage. This remains the primary fertility preservation option for assigned-male-at-birth trans people.
Sperm freezing costs tend to vary, however, Legacy offers three flexible options. Here are Legacy’s sperm freezing costs:
- Yearly Storage: $245
- 5-year storage: $595
Learn more about sperm freezing and sperm freezing costs.
When should a trans woman freeze her sperm?
Estrogen and anti-androgen medications may significantly impair sperm production. Freezing sperm prior to beginning medical transition will typically offer the best results. Trans women and girls can consider sperm freezing options as soon as they hit puberty and are able to produce a semen sample.
However, if you started HRT without preserving your fertility, you still have options. It may be a good idea to start with a semen analysis, to determine whether your hormone protocol has impacted your fertility. If it has, you can take a 3–5 months off of gender-affirming hormone therapy to allow spermatogenesis to resume and sperm quality to improve. A semen analysis is a good first step in the path towards fertility preservation.
Most of the changes to a trans woman’s physical appearance that happen as a result of hormone therapy are not permanent, and stopping cross-sex hormones will lead to reversal. Therefore, taking a pause in feminizing hormones can trigger a trans person’s gender dysphoria and be difficult physically, socially, and emotionally. It may be helpful to work with the support of a gender-affirming counselor or therapist throughout this process.


How much does sperm freezing cost for trans women?
According to LIVESTRONG, the average sperm freezing cost is $1,000, plus $300–$500 per year for ongoing cryogenic storage. In some states, and under some insurance plans, this may be covered for trans women; for many people, though, it’s an out-of-pocket cost.
Part of Legacy’s mission is to increase the accessibility of fertility care and fertility preservation. We offer a few different packages — an analysis package and two options for sperm freezing — that start at $375, with storage that’s less than $200 per year.
See Legacy packages and learn more about sperm freezing costs.
Fertility options when you’re ready to be a parent
If you are a trans woman and you’re ready to be a parent, your options depend on where you are in your transition process, and whether or not you have a partner with a uterus.
Fertility procedures and acronyms defined:
- Intrauterine insemination (IUI): IUI is a process in which a sperm sample, produced via masturbation, is injected through the cervix directly into the uterus at the time of ovulation. Before IUI, the sperm are “washed” to isolate them from the seminal fluid; this step along with giving sperm a “head start” on the fertilization process increases the monthly chance of pregnancy, especially for patients with lower sperm quality.
- In vitro fertilization (IVF): During IVF, egg(s) are retrieved directly from the uterus and fertilized in a lab. The female-bodied partner or egg donor will typically be prescribed hormone medications to prompt their body to produce multiple eggs in one menstrual cycle, increasing the chances that one or more will be healthy and fertilize. The fertilized eggs are monitored as they develop for 3–6 days and then 1–2 are placed into the uterus of a parent or surrogate, where they will hopefully implant and result in pregnancy.
- Intracytoplasmic sperm injection (ICSI): In traditional IVF, the egg and sperm are combined in a lab dish to encourage fertilization. During ICSI, a single sperm is instead injected directly into the egg. This is a helpful procedure for those with severe male-factor infertility such as very low sperm count, motility, or morphology
- Traditional surrogacy: Traditional surrogacy is an arrangement in which the surrogate or “carrier” (the person who carries a pregnancy on behalf of the intended parents) is also the biological parent of the baby, and no egg donor is required. While this arrangement involves fewer expenses than gestational surrogacy (see below), in part because you can use IUI instead of IVF, it’s also more legally complicated
- Gestational surrogacy: During gestational surrogacy, the surrogate or gestational carrier is not genetically related to the baby — the pregnancy is created via IVF with an egg from an intended parent or an egg donor, and sperm from an intended parent or sperm donor.
If you have a partner with a uterus
Options for those who have a penis and testicles and haven’t frozen their sperm:
First, you can do a semen analysis to determine how significantly your hormone therapy has affected your fertility.
If the semen analysis determines you are still producing some healthy sperm, you can attempt to conceive with your partner naturally (via sexual intercourse). Alternatively, you could do an IUI if you want to increase the chances of pregnancy or are not comfortable with penis-in-vagina sex. Sperm freezing is also an option, ensuring you can create a pregnancy later.
If your semen analysis determines you’re not producing healthy sperm, you may be able to recover fertility by stopping hormone therapy for 3–5 months. You could also try IVF with ICSI, which requires only a single healthy sperm and can help achieve pregnancy even when sperm are very few, or motility/morphology is poor.
Options for trans women who have frozen their sperm:
If you have frozen sperm available, you can attempt pregnancy with your partner without stopping your hormone therapy. Frozen sperm can be used in IUI, IVF, or IVF with ICSI, depending on the quantity and quality of the sample once thawed. That’s why sperm freezing is an important consideration for fertility preservation.

If you do not have a partner with a uterus
Surrogacy (gestational or traditional) is an option for you. You can attempt to use a “fresh” semen sample from yourself or your partner — again, you will want to do a semen analysis first to determine if you are producing healthy sperm. Or, if you have frozen your sperm first, you can use it in IUI, IVF, or IVF with ICSI to create a pregnancy with your surrogate’s egg or an egg donor.
Fertility resources for trans women
Considering fertility preservation as a trans person can be an emotional process. It can be difficult to think about all of the options you may want to have in the future, especially if you are starting your transition in your teens or early 20s, when family-building is often not top of mind.
Fertility preservation as well as accessing fertility care such as IUI and IVF is also expensive. Sperm freezing options can lower this cost in the long run.
It may be helpful to seek guidance and support throughout the fertility preservation or treatment process from a trans-affirming therapist or organization.
Euphoria offers a suite of digital apps specifically designed for trans people. Apps include Solace, which gives virtual guidance and information for every step of transition; Bliss, a money management app for those saving for medical transition; and Catharsis, a mental health support platform for the trans community, by the trans community.

Gay Parents to Be is an informational resource for LGBTQ family-building and parenting, including trans parents. This organization offers guidance for those considering fertility preservation pre-transition or hoping to start a family, including mental health support and financial guidance, such as a list of fertility grants and assistance in understanding insurance coverage.

A digital healthcare platform for trans people who want to access hormone replacement therapy and other medications, Folx Health also offers invaluable resources and guidance to patients.
References
- I de Nie et al. “Impaired semen quality in trans women: prevalence and determinants.” Human Reproduction, 2020.
- Courtney Marsh et al. “Low total motile sperm in transgender women seeking hormone therapy.” Journal of Assisted Reproduction & Genetics, 2019.
- R Mieusset et al. “The potential of mild testicular heating as a safe, effective and reversible contraceptive method for men.” International Journal of Andrology, 1994.
- R Mieusset et al. “Hyperthermia and human spermatogenesis: enhancement of the inhibitory effect obtained by ‘artificial cryptorchidism.’” International Journal of Andrology, 1987.
- J C Prior et al. “Spironolactone with physiological female steroids for presurgical therapy of male-to-female transsexualism.” Archives of Sexual Behavior, 1989.
- Federica Di Guardo, et al. “Low Testosterone and Semen Parameters in Male Partners of Infertile Couples Undergoing IVF with a Total Sperm Count Greater than 5 Million.” Journal of Clinical Medicine, 2020.
- F Schneider et al. “Andrology of male-to-female transsexuals: influence of cross-sex hormone therapy on testicular function.” Andrology, 2017.
- Marissa A Kent et al. “Effects of Feminizing Hormones on Sperm Production and Malignant Changes: Microscopic Examination of Post Orchiectomy Specimens in Transwomen.” Urology, 2018.
- Peter Y Liu et al. “Rate, extent, and modifiers of spermatogenic recovery after hormonal male contraception: an integrated analysis.” Lancet, 2006.
- Emily P Barnard et al. “Fertility Preservation Outcomes in Adolescent and Young Adult Feminizing Transgender Patients.” Pediatrics, 2019.