01. The male factor
More than half of men don’t know what’s affecting their fertility.
When it comes to all things fertility, most people think about the woman’s role, and we can’t blame them. Periods, pregnancies, progesterone — it seems like all the conversations focus on just one half of the fertility equation. And our survey reveals a huge male fertility knowledge gap, so we still have some work to do.
But before we even begin talking about the other side of the equation, let’s break down what the science shows when it comes to infertility.
PERCEPTION
Both men and women underestimate the role of the male factor in infertility.
No role?
35% of men and 40% of women underestimated the role that male-factor infertility plays. In fact, 1 in 10 of respondents believed that male-factor fertility plays little to no role in conception.
REALITY
Male-factor infertility is just as likely to be the cause of infertility as female-factor infertility.
The male factor — which includes sperm health and sexual dysfunction — is the sole cause of infertility in about 30% of infertility cases, and contributes to another 20% where both male and female infertility are at play.
KEY TAKEAWAY
Fertility is not just a women’s issue.
All too often, fertility is seen as a “women’s issue.” Sperm health isn’t tested until a couple has been trying to get pregnant for a year, if it’s tested at all.*
In our survey, only 1 in 4 men who were trying to have children had tested their fertility.
This can lead to misinformed medical advice that favors more expensive assisted reproductive treatments, like in vitro fertilization (IVF). In many cases, addressing the male-factor infertility is a much more affordable option.
*Studies show that 1 in 4 infertility consultations doesn’t include a male-factor evaluation. Source: Turner, Katerina A et al., 2020
02. AGE & MALE FERTILITY
Older, wiser… and less fertile?
A combination of social and economic factors have led to an increase in age for many first time parents. The benefits of postponing parenthood include more financial stability, improved partner relationships, and an increase in educational and emotional support for the child.
But unlike wine and cheese, semen quality does not get better with time.
PERCEPTION
Most people aren’t aware that male fertility declines with age or at what age that decline begins.
I can do this forever
70%
70% of respondents overestimated the age at which male fertility decline began, or didn’t know male fertility declined at all.*
*Interestingly, women were more likely to underestimate the impact of age on male fertility: 85% of cisgender female respondents were unaware male fertility decline begins in a man’s 30s.
REALITY
For many, sperm count and quality begins to measurably decline in their late 30s.
One study of patients undergoing IUI found that pregnancy rates for fathers 35+ were less than half what they were for fathers under 35.
As the media broadcasts celebrities in their 50s, 60s, and even 70s becoming dads, it’s easy to see why we may think that’s the norm.
Source: Harris et al. Fertility and the Aging Male (2011)
03. FACTORS AFFECTING MALE FERTILITY
What actually affects sperm health?
Most of us have no idea.
We asked respondents to identify the factors that affect male fertility.
Over half got it wrong.
Masturbation
Perception
Should I hold it?
One quarter (25%) of respondents believed that reducing masturbation — a practice known as semen retention — can benefit fertility health.
Reality
Don’t be afraid to let it out
There’s no scientific evidence that semen retention improves fertility. In fact, cutting back on masturbation can actually be detrimental to sperm and prostate health as sperm motility drops while it sits in storage.
Varicocele
Perception
Varico-what?
Only 9% of respondents identified varicocele as a factor affecting male fertility.
Reality
One of the most common, least known causes of male-factor infertility
Varicocele, swollen veins in the testes, are present in about 40% of cases of male-factor infertility. Despite how prevalent it is in cases of male-factor infertility, less than 1 in 10 respondents could identify it.
Source: UCLA Health. Varicocele: Symptoms, Treatment, Diagnosis
Occupation
Perception
Separating work and personal life
Understandably, most people don’t associate their work with their fertility. Only 14% of respondents identified occupation as a factor affecting male fertility.*
*Awareness among men in high-risk industries, such as agriculture, manufacturing, and the military, was only slightly higher: 17%.
Reality
Where the line gets blurry
Certain jobs that involve exposure to chemicals or toxins or increase risk of injury — including police officers, night shift workers, and military members — can significantly increase a person’s chance of infertility. For example, some studies showed that veterans and members of the military are twice as likely to experience infertility compared to civilians.
Source: Katon et al. Self-reported infertility among male and female veterans serving during Operation Enduring Freedom/Operation Iraqi Freedom (2014).
Environmental exposures
Perception
Out of sight, out of mind
Unless you live in a smoggy city, you probably can’t see the pollutants that are in the air. As a result, many of us don’t realize the impact our environment has on our fertility. In our survey, only 18% of respondents identified pollution as a factor affecting male fertility.
Reality
It’s all around us all the time
Environmental factors, such as air quality, and exposures to certain chemicals, such as phthalates and bisphenols (BPAs, BPFs, BPSs), are significant contributors to fertility issues. One study showed that, for every 10 μg/m3 increase of particulate matter in the air, exposed couples were 20% more likely to experience infertility.
Sources: Hlisníková et al. Effects and Mechanisms of Phthalates’ Action on Reproductive Processes and Reproductive Health: A Literature Review (2020); Li et al. Association between exposure to airborne particulate matter less than 2.5 μm and human fecundity in China (2021).
Sleep
Perception
Just 10 more minutes, then I’ll go to bed
We’ve all been there. It’s almost too easy to keep scrolling when it comes time to go to bed. But can staying up late really affect your fertility? Only 1 in 4 respondents from our survey thought so.
Reality
You don’t want to mess with the (sleep) cycle
Sleep plays an important role in regulating many bodily processes and is essential for good health. Research shows that late bedtimes and not getting enough quality sleep are correlated with lower sperm count, motility, and survival.
Source: Liu et al. Sleep Deprivation and Late Bedtime Impair Sperm Health Through Increasing Antisperm Antibody Production: A Prospective Study of 981 Healthy Men (2017).
Alcohol
Perception
They say that red wine is good for your heart… but what about for your sperm?
Many people turn to alcohol for socialization and as a way to relax after a long day of work. But not so many people think about the impact alcohol has on fertility. Only 43% of respondents identified it as a factor in male fertility.
Reality
Think before you drink
Research has shown that drinking alcohol can have an impact on reproductive hormone levels. One study found that consuming more than five drinks per week can be detrimental to sperm count and morphology. Regular drinking was also associated with lower sperm quality.
Source: Jensen et al. Habitual alcohol consumption associated with reduced semen quality and changes in reproductive hormone changes (2014).
Smoking and cannabis
Perception
Cigarettes are bad for your lungs and gum health, but is that it?
Many people overlook the impact that smoking has on the body holistically. And despite the rise of recreational and medicinal marijuana, not many people think about the detrimental effects of weed.
From our survey, 47% of respondents identified smoking as a factor affecting male fertility. Meanwhile, only 28% identified cannabis as a factor.
Reality
Puff, puff… pass?
The American Society of Reproductive Medicine considers cigarette smoking one of the leading risk factors for infertility. Men who smoke are about twice as likely to experience infertility, compared with non-smokers. Meanwhile, most studies show that regular cannabis use is negatively associated with fertility and semen parameters.
Sources: American Society for Reproductive Medicine. Smoking and infertility: a committee opinion (2018); Payne et al. Cannabis and Male Fertility: A Systematic Review (2019)
Saunas and hot tubs
Perception
Can a dip in the hot tub really lead to a dip in fertility?
Only 21% of respondents identified the use of hot tubs and saunas as a factor affecting male fertility. After all, your semen quality is probably the last thing you’re thinking about before getting in a hot tub.
Reality
Pay attention to those time limits
Saunas and hot tubs overheat the scrotum, potentially affecting sperm production for months after use. Higher temperatures can also lead to oxidative stress, which can damage the DNA inside the sperm.
Underwear
Perception
Boxers vs. briefs, does it really matter?
1 in 3 respondents identified “underwear choice” — i.e., the boxers vs. briefs debate — as a significant factor in male fertility.
Reality
No need to get your boxers in a bunch
Despite tons of pop culture attention to this issue, the evidence is mixed. Undergarments that hold the scrotum snug against the body increase the temperature at which the sperm is stored and can impact sperm quality, but for many people, their choice of underwear will likely not have a detrimental impact on their sperm health.
04. HORMONE THERAPY
Is more testosterone really the answer?
Almost everyone misunderstands how hormone therapy affects fertility — including those currently taking hormone therapy.
Testosterone is the primary hormone associated with masculinity. And masculinity is so often tied to fertility. So it’s no surprise that most people assume more testosterone equals more fertility.
But the reality is much less simple. There are many fertility hormones at play and external sources of testosterone can create an imbalance, often leading to infertility.
PERCEPTION
There are some big misconceptions about hormone therapy.
Not so yolked
72%
72% of respondents believed that taking testosterone would improve a person’s fertility.
Even more shocking, nearly ¾ of men taking testosterone replacement therapy (TRT) right now aren’t aware of its effect on their fertility.
Goodbye fertility
27%
In our survey, only 27% of cis men taking testosterone were aware that their fertility may not return for 3–6 months or more.
Unnecessary challenges
18%
18% of cis men taking testosterone were trying to have kids at the same time.
We found a similar pattern among trans folks who were taking gender-affirming hormone therapy (GAHT).
Futureproof?
71%
71% of respondents taking GAHT were unaware of the potential long-term effects on their fertility.
REALITY
Testosterone and estrogen can both impact fertility — maybe even permanently.
One study found that 65% of men on TRT become temporarily sterile within 4 months of use (depending on the dose, the duration, and the baseline semen production).
Gender-affirming hormone therapy — namely estrogen and androgen blockers — can suppress fertility, even permanently. In one study, 1 in 3 trans women did not recover fertility, even after pausing estrogen therapy for 6 months.
As a result, the best time to pursue fertility preservation is before starting GAHT.
Sources: Patel et al. Testosterone Is a Contraceptive and Should Not Be Used in Men Who Desire Fertility (2019); Liu et al. Rate, extent, and modifiers of spermatogenic recovery after hormonal male contraception: an integrated analysis (2006).
KEY TAKEAWAY
Education is critical
With TRT on the rise as a trending treatment for symptoms like lack of muscle tone, fatigue, and low sex drive, online testosterone purveyors have made it easy for young men to access a prescription — sometimes without even testing testosterone levels beforehand.
Everyone on TRT needs to understand the long-term impact that treatment can have on their fertility. As testosterone therapy becomes more accessible and TRT usage grows, an increased focus on education must follow.
The good news
We’re seeing increased access to gender-affirming hormone therapy, including virtual care providers. This is hugely net positive for trans patients — medical transition has been shown to significantly improve mental health for those seeking it. As the quality of care improves, we must consider all the opportunities to give trans folks the information they deserve about their future family-building options from the start.
05. VASECTOMY
The truth about vasectomies
They’re getting more popular, but we need to combat misinformation.
The implementation of abortion and birth control restrictions nationwide has increased interest in vasectomy as a highly effective, permanent male birth control option.
As female birth control options face legal scrutiny, some are considering male birth control options as alternatives.
Political snips
20%
20% of respondents reported that they or their partner has considered, planned, or gotten a vasectomy as a response to the overturn of Roe v. Wade.
We love to see cis men getting more involved in family planning. But it seems like we’re still not communicating some important facts about vasectomies.
PERCEPTION
Despite some misconceptions, vasectomy reversals are not always successful.
Uno reverse!
35%
35% of respondents believed that vasectomy reversal was guaranteed to recover fertility.
REALITY
Pregnancy rates after vasectomy reversals can be as low as 30%.
Getting a vasectomy reversal — which requires a more invasive surgical procedure, weeks of recovery, and has no guarantee of success — is not as easy as the initial snip. Pregnancy rates after vasectomy reversals can be as low as 30%, depending on several factors, including how long it’s been since the initial vasectomy. So think twice before you make a final decision.
KEY TAKEAWAY
Vasectomy patients need more education
Less than 10% of the respondents who had gotten or were planning a vasectomy had frozen their sperm.
Life happens. So even if you’re super sure about your decision to get the snip, why not safeguard your options for later? Sperm freezing prior to a vasectomy protects your fertility and can improve your chances of having a biological child if circumstances change in the future.
06. CURRENT EVENTS & FERTILITY
Potential parents are feeling the pressure of a pandemic and a looming economic recession.
We live in a precarious time. Health and economic uncertainty are at the forefront of many people’s minds and, as a result, many are choosing to wait to start a family.
Delaying the timeline to parenthood is a decision that is often influenced by economic and social factors.
Going child-free?
25%
1 in 4 respondents put off having kids or decided not to have children at all due to the COVID-19 pandemic.
Economic cuts
30%
1 in 3 respondents say they’ll have fewer children, have children later, or won’t have children at all as a result of the current economic situation.
Why does this matter?
We are already at a record low in terms of fertility rates — and a record high in terms of parental age.
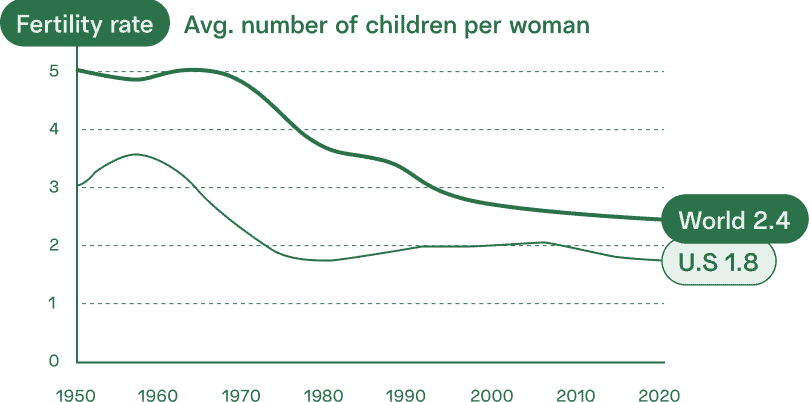
We know that age affects both male and female fertility. If those who want kids put off starting their families for even longer, we could be facing a crisis of widespread infertility, smaller family sizes, and necessity for assisted reproductive technology.
KEY QUESTION
How can we as a society better support those who want children?
KEY QUESTION
Consider:
Increasing education about the role of male-factor infertility
Advocating for male fertility conversations in healthcare spaces
Normalizing sperm freezing just as much as egg freezing
07. FERTILITY BENEFITS
Most people think fertility coverage is important, but they may not know they have it.
Socioeconomic status should not dictate the fertility options that are available to you. Expanding access to fertility services through employer benefits is an important step to increasing the accessibility of fertility treatments.
But fertility employer benefits are still, by most measures, an uncommon offering.
Only about 1 in 3 respondents who were employed full-time reported that their companies offered coverage for fertility testing and treatment.
Despite the relatively low rate at which fertility benefits are offered, it is clear that this is a valued benefit that many employees consider when making employment decisions.
Show me the money
1 in 3
1 in 3 respondents say fertility benefits would be likely or extremely likely to sway their employment decisions.
For her…
55%
55% believed it was important for employers to offer female fertility benefits.
…and for him
50%
50% believed it was important for employers to offer male fertility benefits.
KEY TAKEAWAY
Top benefits attract top talent
But the companies that do offer fertility coverage need to do more to communicate these benefits clearly, in recruitment materials employee engagement efforts, to attract and retain their best employees.
More than 1 in 3 respondents (34%) weren’t sure if their employer offered fertility benefits.
CONCLUSION
Let’s empower men to take an active role in their part of the fertility equation.
The societal emphasis on a woman’s role as a caregiver and parent has created an imbalance in how we think about fertility.
But the data is clear: This is not just a woman’s issue.
As this report has reviewed, there are many factors that can lead to a decline in male fertility and many ways to minimize the risk — most people just don’t know. Expanding how we think about fertility issues, by considering ways to prevent and address male-factor infertility, opens the door for more holistic and cost-effective methods of addressing family-building challenges.
It’s about time that we invite all men — our friends, brothers, and sons — into the conversation.
Taking action starts with building awareness of testing, treatment, and freezing options.
At-home sperm testing
Learn more about your fertility by taking an at-home sperm test with clinic-grade accuracy.
This report was created in a partnership between Legacy and Carrot Fertility.
Carrot Fertility is the leading global fertility care platform for women, who are often at the center of fertility care decisions and consequences. Plus, Carrot serves people of every age, race, income, sex, sexual orientation, gender, marital status, and geography.
Learn more at carrotfertility.com.
Legacy is America’s largest at-home fertility clinic for people with sperm, empowering individuals to learn more about their sperm health and fertility with secure and private testing and freezing options. Partnerships with leading health plans, fertility benefits providers, U.S. military programs, and financing merchants make industry-leading sperm testing and freezing options affordable and accessible.
Learn more at givelegacy.com.

