The journey to parenthood isn’t always as clear-cut as it’s made out to be. Approximately 9% of men in the US have reported seeking advice, testing, or treatment for infertility. While many cases of male-factor infertility can be treated with simple lifestyle interventions, in some cases, the cause is deeper — your genes. Read on to learn about the genetic causes of male-factor infertility, and the different types of genetic infertility.
Key takeaways
- There are a few known, but rare genetic conditions that affect male fertility or cause male-factor infertility.
- In general, the impact of genetics on male fertility is not fully understood. Genetics may contribute to anywhere from 15–60% of male-factor infertility.
- Many causes of genetic male infertility can be overcome with assisted reproductive technology (ART), or fertility treatments.
What is male-factor infertility?
Infertility is a condition in which a couple or a person isn’t able to conceive a healthy pregnancy within 6–12 months of actively trying. Male-factor infertility refers to difficulty conceiving that’s primarily caused by issues with the sperm’s inability to fertilize the egg. A number of conditions could contribute to male-factor infertility, including low sperm count or poor sperm motility.
In cases of sole male-factor infertility, the female partner is fertile, and has properly functioning ovaries, fallopian tubes, and uterus. Female-factor infertility would be the opposite — a case in which the male partner was fertile, but the female partner had a condition that affected their ability to conceive or carry a pregnancy.
Experts estimate about one-third of infertility cases are male-factor infertility, one-third are female-factor infertility, and the final third involve factors related to both partners, or are unexplained. Male fertility testing is the most effective way at diagnosing the root cause of your infertility.
How common is genetic male infertility?
Some experts estimate that 10–15% of male infertility cases are caused by genetics — others calculate it’s more like 60%. So while other male fertility factors like age, diet, lifestyle, and hormones may be common, genetics is sometimes a factor or even the sole cause of male-factor infertility.
Can male infertility be inherited?
One sign that male-factor infertility may involve genetics: There is some evidence that men who are infertile are more likely to have sons who are infertile, as well. One study found that the male children of men who used intracytoplasmic sperm injection (ICSI) to conceive were significantly more likely to experience poor semen quality parameters — including lower sperm concentration, sperm count, and motility — compared to male children who were naturally conceived.
There wasn’t conclusive evidence to pinpoint exactly what caused the low quality semen parameters. They did find that there was no difference across measurements of BMI, smoking, alcohol consumption, or drug use, so lifestyle factors that may be carried from father to son weren’t relevant to this study.
The most likely reason for this correlation is underlying genetics, and not the ICSI procedure itself. Since ICSI is a treatment that helps overcome male-factor fertility issues, such as oligospermia (low sperm count), it’s possible that those same male fertility issues may be genetically passed down to male offspring.
This evidence is backed up by a larger study from 2007 of male children conceived through any type of fertility treatment. Nearly 2,000 young men submitted semen analyses for study. It was found that offspring conceived through fertility treatment had, on average, lower sperm concentration and fewer motile and morphologically normal sperm.
Researchers again concluded that the findings did not “necessarily indicate that female infertility treatment induces a risk of reproductive problems for the next generation,” but “could, in fact, be due to genetic factors inherited through the mother or even the father.”
Genetic causes of male-factor infertility
While genetic factors for lower semen parameters are still research-in-progress, in some rare cases, we can identify a clear genetic cause for male-factor infertility. There are a variety of possible genetic causes for male-factor infertility, including cystic fibrosis, Y-chromosome microdeletions, and Klinefelter syndrome.
Y-chromosome microdeletions and male fertility
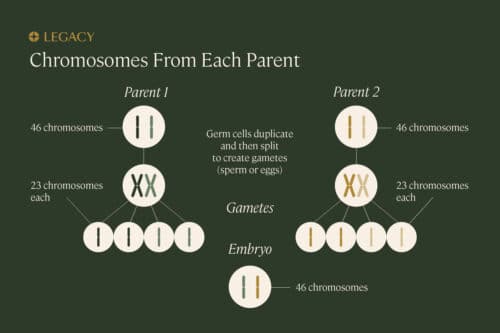
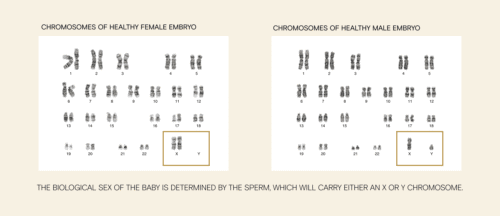
Everyone is born with a set of sex chromosomes; females typically have two X-chromosomes and males have one X-chromosome and one Y-chromosome. The Y-chromosome contains between 50 and 60 genes, and since it’s the male-determining chromosome, many of those genes are specific to the male sex.
For instance, there’s the SRY gene, which causes testes to form in the embryo and results in the development of male genitalia. There are other genes, such as DAZ, RBMY, and BDY, that relate to male fertility factors.
As the name “Y-chromosome microdeletion” suggests, this chromosomal abnormality involves small deletions of genes on the Y-chromosome. Microdeletions of pertinent fertility genes are one possible cause of azoospermia, a condition where sperm is absent in semen, or other male-factor infertility issues.
In a study that observed 200 infertile men and 200 fertile men, it was found that Y-chromosome microdeletions were present in 7% of infertile men, compared to just 2% of fertile men. Of the infertile men with Y-chromosome microdeletions, 9 had azoospermia or severe oligospermia, 4 had oligospermia, and 1 had normal sperm count.
Another study that observed 38 infertile men with microdeletions found that 21% of those men also had another possible cause of male infertility. This data suggests that while the occurrence of Y-chromosome microdeletions tends to be more significant in infertile men, it may not be the only male fertility factor at play, and it doesn’t rule out the possibility of conception.
Cystic fibrosis and male fertility
Cystic fibrosis (CF) is what’s known as a “single gene disorder,” a condition that’s caused by one specific gene. In the case of CF, a mutation in the CFTR gene — if inherited from both parents — changes the expression of a protein that regulates the movement of salt in and out of cells, causing the lungs to fill up with mucus, trouble breathing, and digestive issues.
CF typically also causes congenital absence of the vas deferens, the tube that connects the epididymis (where sperm is stored) to the ejaculatory ducts. This means that men with CF may produce healthy, strong sperm, but lack the connection that carries that sperm to the semen. In fact, 90% of men with CF have normal, healthy sperm production.
Almost all men with cystic fibrosis (CF) are infertile, but can still have biological children with the help of assisted reproductive technology. Procedures like testicular sperm extraction (TESE), paired with IVF, can make fathering biological children possible for patients with CF.
Interestingly, recent studies have revealed that it’s not only those with cystic fibrosis that can experience the effects on their fertility. Cystic fibrosis carriers, those who have inherited the CF gene from one parent, are also at a significantly higher risk for male infertility.
Learn more about cystic fibrosis and male-factor infertility.
Klinefelter syndrome and male fertility
In Klinefelter syndrome, instead of having the typical XY chromosome pair, a male is born with an extra X chromosome (Klinefelter is sometimes referred to as XXY syndrome). Since this condition doesn’t affect day-to-day life, it’s not uncommon for a male to go undiagnosed for most of his life, until assessing male fertility factors.
Klinefelter syndrome is one of the most common chromosomal abnormalities affecting male-factor infertility, and is also one of the most common causes of azoospermia. In fact, Klinefelter syndrome is found in 11% of cases of azoospermia.
Nearly 50% of men with Klinefelter syndrome experience low testosterone levels, and approximately 95–99% of men with KFS experience infertility due to low sperm count. However, this doesn’t necessarily mean that sperm production is absent altogether — sperm is found in more than 50% of men diagnosed with KFS.
Studies have found benefits to sperm freezing for men with Klinefelter syndrome, and recommend this as an option to young males diagnosed with this genetic form of male-factor infertility.
Learn more about Klinefelter syndrome.
46 XX syndrome and male fertility
46 XX is a rare condition in which a person is born with the XX chromosome typically found in females, but is also born with external male genitalia. This condition occurs in 1 out of every 20,000–25,000 newborns assigned male at birth, and is an intersex condition.
While the physical manifestation of this condition varies, people with 46 XX will typically experience underdeveloped genitalia and azoospermia. Chances of biological parenthood with this condition are incredibly slim. Since 46 XX is such a rare condition, patients with 46 XX currently make up less than 1% of male-factor infertility cases.
Primary ciliary dyskinesia/Kartagener’s syndrome and male fertility
Kartagener’s syndrome is one of a family of diseases known as primary ciliary dyskinesia (PCD). PCDs are rare inherited diseases that impact the cilia — tiny, hair-like structures — that line internal airways. As a result, the most common symptoms are chronic respiratory infections, abnormally positioned internal organs, and male-factor infertility.T
he epididymis, a series of tubes where sperm is stored, is lined with cilia-like structures that help sperm cells move. Since PCD affects cilia and cilia-like structures, sperm cells may not be able to effectively travel. In addition, motile cilia and sperm flagella (tails) share common structures, so many patients with PCD experience severe or total asthenozoospermia (sperm with reduced or no motility). Approximately 75% of men with Kartagener’s syndrome experience male-factor infertility.
Kallmann syndrome and male fertility
Kallmann syndrome is a rare condition affecting 1 out of every 30,000 males, causing delayed or absent puberty. Kallman syndrome causes a lack of hormones that direct sexual development, which is why it is most commonly diagnosed during adolescence. Although other symptoms, like impaired sense of smell are prevalent in those with Kallmann syndrome, it is usually delayed puberty that alerts a doctor’s attention, provoking testing and diagnosis.
Most males with this condition experience absent sperm production and male-factor infertility. In some cases, sperm production can be induced by long-term administration of GnRH, which is a hormone that causes the pituitary gland in the brain to make and secrete male fertility hormones like luteinizing hormone (LH) and follicle-stimulating hormone (FSH) to stimulate testosterone and sperm production.
Who should consider genetic testing for infertility?
When testing for male fertility, genetic testing is typically performed after frontline tests like semen analysis and sperm DNA fragmentation analysis. If you’ve gone through rounds of fertility testing or have a unique family medical history, genetic testing may be your next step.
The following people should consider genetic testing:
- Those who have a family history of a condition like cystic fibrosis
- Those who have had a child with a genetic or chromosomal condition
- Those experiencing male-factor infertility as diagnosed with one or more semen analysis tests
Genetic testing is typically done with a simple blood test. From there, a lab can analyze your genetic code to detect any abnormalities that may affect male-factor infertility or the health of your child. Genetic testing is often recommended while trying to get pregnant, or before you start planning to conceive.
Learn more about genetic testing for infertility.
Genetic male infertility versus sperm DNA fragmentation
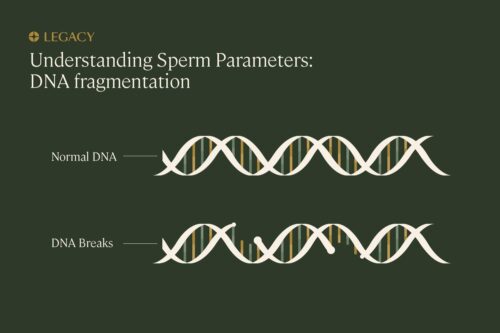
Sperm DNA fragmentation may sound like it’s related to genetics, but inherited infertility and sperm DNA fragmentation are two very different things.
Genetic infertility is inherent at birth (or “congenital”), such as in the above cases, where an aspect of your chromosomal genetic makeup experienced a mutation. Sperm DNA fragmentation, on the other hand, is damage specifically to the DNA inside the sperm cells, usually brought on by age, smoking, illness, infection, or environmental toxin exposure. This damage can occur at multiple points in the sperm’s lifecycle, from production in the testes to when it’s in “storage” in the epididymis or even post-ejaculation.
While genetic testing will typically require on-site clinic visits, there is an at-home sperm DNA fragmentation analysis kit that makes male fertility factor testing easier.
Other causes of male-factor infertility
While male fertility can be impacted by genetics, there are other common male fertility factors that you may want to consider if you’re having trouble conceiving. These include:
- Age. Although those who produce sperm can usually do so throughout their entire lifetime, that doesn’t mean that the quality of sperm remains constant. Sperm quality parameters naturally decline with age, and most people see a significant decline in sperm motility after the age of 40. Studies also show that DNA fragmentation becomes more common with age.
- Diet and exercise. Research shows that there’s an association between male-factor infertility and obesity. Diets high in fried foods, refined grains, added sugars, and processed meats correlate with poor male fertility factors, like reduced sperm count, motility, and morphology. Exercise regimens such as walking and jogging have been shown to improve fertility markers. Learn more about sperm improvement.
- Alcohol and tobacco consumption. Smoking cigarettes and excessive alcohol consumption can affect all aspects of male fertility, from sperm concentration to count, motility, and morphology. Reducing your alcohol intake to less than five drinks per week and quitting smoking are both great ways to improve your fertility.
- Lack of sleep. Not enough quality sleep may contribute to male-factor infertility. Research shows that getting less than 7–8 hours of uninterrupted sleep is associated with lower total motility, sperm count, and morphology.
How can I check my own fertility?
If you’re trying to conceive, suspect or know you have a genetic condition affecting male fertility factors, or have a family history of male-factor infertility, sperm testing is a great place to start.
Legacy’s at-home semen analysis kits allow you to test for crucial sperm parameters — sperm count, motility, and concentration — from the comfort of home. We offer the most scientifically advanced at-home semen test, with the option to add sperm DNA fragmentation analysis as well. Our sperm testing is conducted in CLIA-certified labs by a team of experienced scientists, and all results are reviewed by our medical staff.



