Whether to have a vasectomy is a big decision that comes with a number of smaller decisions. One of these is which type of the vasectomy to have — scalpel vs. no-scalpel vasectomy.
Here, we’ll explore the step-by-step differences between a scalpel vs. no-scalpel vasectomy, the recovery time for each, and what makes someone a candidate for a no-scalpel vasectomy.
Key takeaways
- There are two main types of vasectomies: the incision method (AKA “scalpel vasectomy” or “traditional vasectomy”) and no-scalpel vasectomy.
- Both versions of the procedure are performed under local anesthesia and take about 20 minutes.
- No-scalpel procedure is considered less invasive and has a shorter recovery time. However, not every patient is a candidate.
- All vasectomy patients should consider freezing sperm beforehand, and should do a semen analysis about 3 months after their vasectomy to ensure the procedure was successful.
Scalpel vasectomy vs. no-scalpel vasectomy
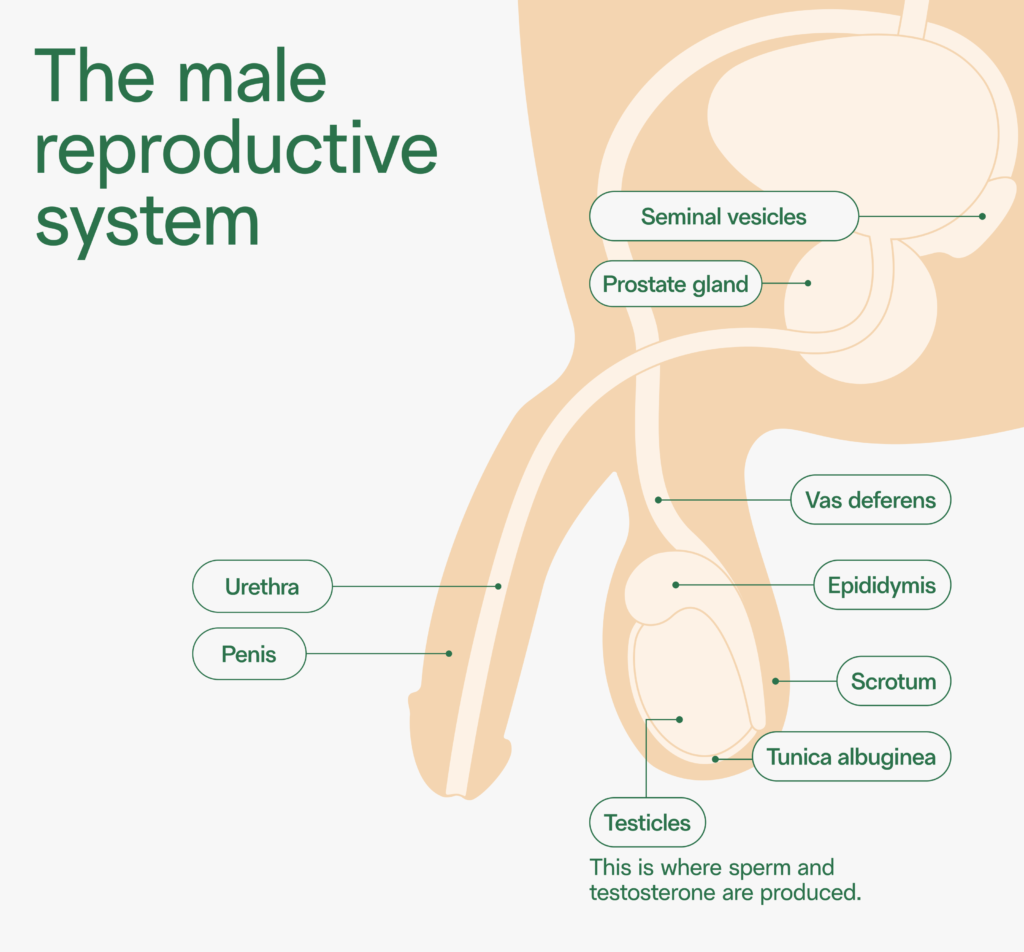
A vasectomy is a form of surgical, permanent male birth control. During a vasectomy procedure, the vas deferens (the tubes behind each testicle) are severed by a doctor and the ends are sealed.
A vasectomy prevents sperm, which are produced in the testicles, from mixing with semen. After a vasectomy, a person can still ejaculate, but their semen will contain no sperm.
Learn more about how a vasectomy works.
There are two main types of vasectomies:
- Incision method. Often known as “traditional” or “conventional” vasectomy, in this method, a surgeon will make one or two small incisions in the scrotum with a surgical scalpel in order to reach the vas deferens.
- No-scalpel method. In a no-scalpel vasectomy, the surgeon uses a sharp instrument to punch a small hole in the scrotum, then gently stretches the skin to access the vas deferens.
| Traditional vasectomy vs. | No-scalpel vasectomy | |
| Anesthetic | Numbing injection | Numbing injection or jet spray |
| Process | 1–2 small incisions in the scrotum. Surgeon will cut both vas deferens, then cauterize or tie the ends. | 1–2 punctures in the scrotum, then the skin is stretched. Surgeon will cut both vas deferens, then cauterize or tie the ends. |
| Surgical closure | Stitches or glue | May heal without closure or sutures |
| Surgery time | 24 minutes on average | 20 minutes on average |
| Chance of side effects & complications | Slightly more likely (but still very uncommon) | Slightly less likely |
| Candidates | Nearly anyone | May not be an option for those with vas deferens that are difficult to palpate, or those with varicocele or hydrocele |
| Success rates | 99+% effective | 99+% effective |
Both procedures are performed under local anesthesia — usually an injection of lidocaine to numb the area. In most cases, this is the only pain the patient will feel.
In what is called a “no-needle, no scalpel” vasectomy, the lidocaine is delivered to the surgical area through a high-pressure jet spray instrument. The patient will still feel mild discomfort; some say it’s similar to a rubber-band snap or mosquito bite.
In all versions of the procedure, the lidocaine kicks in within a few seconds. The procedure itself takes about 20 minutes.
The incision area is sealed with sutures or surgical glue. In some cases, the no-scalpel incision can heal on its own.
Which vasectomy is less painful? Which has a shorter recovery time?
Which vasectomy is best? That depends on your criteria. The no-scalpel procedure is considered the least invasive vasectomy and has a shorter recovery time — a few days. The recovery time for a traditional vasectomy is about a week.
No-scalpel vasectomies are generally considered slightly less painful. According to a recent study, 36% of patients report feeling discomfort during a vasectomy. Those numbers are slightly higher for traditional vasectomy patients (40%) than no-scalpel vasectomy patients (33%).1
And according to a 2014 review of research, no‐scalpel vasectomies are accompanied by less bleeding, bruising, infection, and pain, and a shorter operation time than traditional vasectomies.2
After the operation, any discomfort is generally managed with acetaminophen (brand name Tylenol) and ice. Overall, 95% percent of vasectomy patients are pain-free starting two weeks after the procedure.1
Learn more about pain during and after vasectomy.
Which form of vasectomy is more effective?
What is the success rate of a no-scalpel vasectomy? Both versions of the vasectomy have the same result: the severing of the vas deferens for permanent birth control. Studies have found that, for those who are good candidates, no-scalpel vasectomy is as effective as traditional vasectomy.2
Overall, vasectomies are one of the most effective forms of contraception. According to the American Urological Association (AUA), vasectomy has a 0.05% (1 in 2,000) chance of failure.3
For comparison, the failure rate of condoms is 1 in 100 uses, and the failure rate of tubal ligation (women getting their “tubes tied”) is 1.85 in 100 cases.
Learn more about the chance of vasectomy failure.
How to choose scalpel vs. no-scalpel vasectomy
First, it’s most important that you speak to your urologist to understand if you’re a good candidate for no-scalpel vasectomy.
Most men are good candidates for a no-scalpel vasectomy. But If your anatomy is complicated — for example, if a doctor can’t feel both vas deferens or if you have large hydroceles or varicoceles or past scarring of the scrotum — you may not be an ideal candidate for a no-scalpel vasectomy and may need to undergo the traditional form of the procedure instead.
But that is rare. One group of New York urologists reported that more than 95% of men are able to have a no-scalpel vasectomy.4
Comparing costs of no-scalpel vasectomy
Both a conventional and a no-scalpel vasectomy cost about the same — $800–$2,000, depending on who performs the surgery and where it’s done. In most cases, health insurance covers vasectomy, regardless of the method used.
Tips for a successful vasectomy
Here’s your checklist for a successful vasectomy:
- Freeze your sperm before a vasectomy, in case you change your mind about having children in the future. (It happens — about 10% of the time.) This is a more effective and affordable backup plan than vasectomy reversal.
- Plan to take one to two days off from work after your vasectomy.
- Wear supportive underwear for about a week after the procedure.
- Stock up on ice and acetaminophen to manage discomfort.
- Get a semen analysis about 3 months after your vasectomy to determine that no sperm remain in your semen. Use back-up birth control until you get the all-clear.
Resources
- 1. Sokal et al, 1999. “A comparative study of the no scalpel and standard incision approaches to vasectomy in 5 countries.”
- 2. Cook et al, 2014. “Scalpel versus no‐scalpel incision for vasectomy.”
- 3. Sharlip et al, 2012. “Vasectomy: AUA Guidelines.”
- 4. Shteynshlyuger, Alex. “No scalpel vasectomy: Who is a good candidate?”



