What options do you have if your sperm concentration is low, if there’s no sperm in your semen, or if you struggle with ejaculating? Let’s learn more about testicular sperm retrieval, who could benefit from these male fertility treatments, and how testicular sperm extraction could boost IVF and ICSI success.
Semen does not always equal sperm. If you’re scratching your head at that statement, you’re not alone. Many people are surprised to learn that around one-third of infertility cases tie back to male-factor infertility — with lack of sperm in semen (the fluid that carries sperm to the egg) being one of the biggest roadblocks.
Key takeaways
- Testicular sperm retrieval makes IVF and ICSI treatments possible for people with no sperm in their semen or those who cannot ejaculate.
- Testicular sperm extraction and testicular sperm aspiration options are available to fit specific needs, medical conditions, and preferences.
- For people who have gotten a vasectomy and didn’t do sperm freezing beforehand, testicular sperm retrieval offers a path to get pregnant without reversing the vasectomy.
What is testicular sperm retrieval?
Testicular sperm retrieval is a procedure in which a doctor pulls sperm from the testicles, using a needle or scalpel, instead of through a semen sample. For people who struggle with ejaculation or learn their sperm concentration is low or they have azoospermia (no sperm in their semen), testicular sperm retrieval may be a step in in-vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).

How can testicular sperm retrieval benefit male fertility?
Testicular sperm retrieval gets sperm directly from where it’s produced and stored: the testicles. For some patients, sperm retrieved from the testes may be more plentiful or better quality, or may allow them to bypass a blocked or absent vas deferens (the tubes that carry sperm out of the testes).
Testicular sperm retrieval may be an option for those with:
- Lack of sperm in the semen (azoospermia)
- Low sperm count or low sperm concentration
- Poor sperm motility, morphology, or DNA fragmentation
- Congenital absence of the vas deferens
- Ejaculatory or erectile dysfunction
- Vasectomy or unsuccessful vasectomy reversal
- Genetic male infertility
For people who have struggled to conceive naturally, testicular sperm retrieval may make fertility treatments like IVF or ICSI possible. Let’s dig a little deeper into the ways testicular sperm retrieval could benefit male fertility patients.
Testicular sperm retrieval for people with absence of the vas deferens
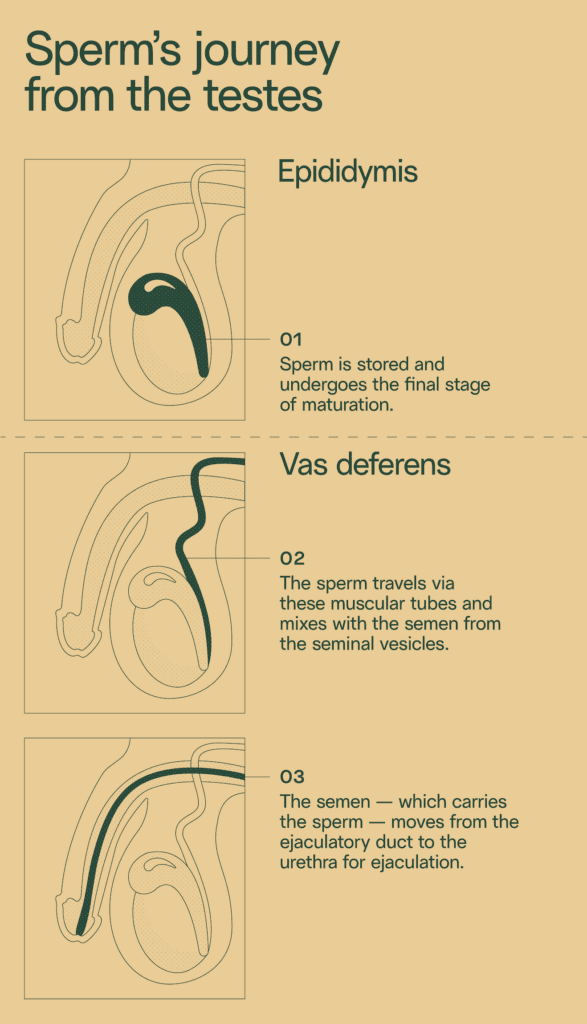
About 0.1% of people with testes are born without both vas deferens. These are the muscular tubes that carry sperm from the epididymis (where sperm is stored in the testicles) to the ejaculatory ducts, where they’re mixed with semen and ejaculated from the penis.
People without either vas deferens are typically perfectly capable of producing healthy sperm, but lack the “plumbing” to transport the sperm out of their testicles. Therefore, they may be diagnosed with azoospermia after a semen analysis.
Testicular sperm retrieval bypasses the need for the vas deferens.
Testicular sperm retrieval for people with poor semen parameters
For some, low semen parameters, such as sperm count, motility, genetic health, or morphology, is their infertility culprit. Symptoms of male infertility can be caused by genetic abnormalities, blockages in the vas deferens or other parts of the reproductive system, injuries to the penis or testicles, or hormone imbalances.
Depending on your male-factor infertility diagnosis, it may be easier to find healthy sperm by going directly to the source — the testes. With testicular sperm retrieval, a doctor can retrieve viable sperm for in-vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
Testicular sperm retrieval after vasectomy or failed vasectomy reversal
Vasectomy is a permanent birth control option. During a vasectomy, the tubes that carry sperm to the penis are cut and sealed to block sperm from reaching the semen. While vasectomies can be reversed, the procedure is not 100% guaranteed. That’s why experts recommend freezing sperm prior to vasectomy.
If you haven’t frozen any sperm, and you don’t want to undergo vasectomy reversal — or your vasectomy reversal didn’t work — you may turn to testicular sperm retrieval. Even after a vasectomy, your testes typically continue to produce some healthy sperm. Testicular sperm retrieval makes pregnancy possible without vasectomy reversal or if a reversal was unsuccessful.
Testicular sperm retrieval before medical treatment
While bettering or even extending a person’s life, many medical treatments can impact male fertility. The ASRM lists some of the most impactful: cancer treatments, finasteride treatment, gender-affirming treatment, and certain surgeries.
Typically, sperm freezing would be the first choice for these patients. However, in some situations, patients may not be able to achieve erection or ejaculation in order to freeze sperm in the conventional way. Sperm retrieval gives these patients the choice to freeze sperm at its healthiest before undergoing one of these treatments.
Testicular sperm retrieval for people with ejaculatory dysfunction
The most common form of ejaculatory dysfunction is premature ejaculation. In fact, the Urology Care Foundation reports that around 1 in 3 men between the ages of 18 and 59 struggle with it.
Some other common types of ejaculatory dysfunction include:
- Retrograde ejaculation. Colloquially called a “dry orgasm,” retrograde ejaculation happens when semen flows back into the bladder instead of out of the penis.
- Delayed ejaculation. People with this dysfunction either struggle to orgasm in a timely manner or at all.
By going directly to the source, testicular sperm retrieval removes the pressure to ejaculate at the “right time.”
Testicular sperm retrieval procedures
When ejaculation isn’t the simplest way to find sperm, these five sperm retrieval techniques offer options for creating a pregnancy with IVF.
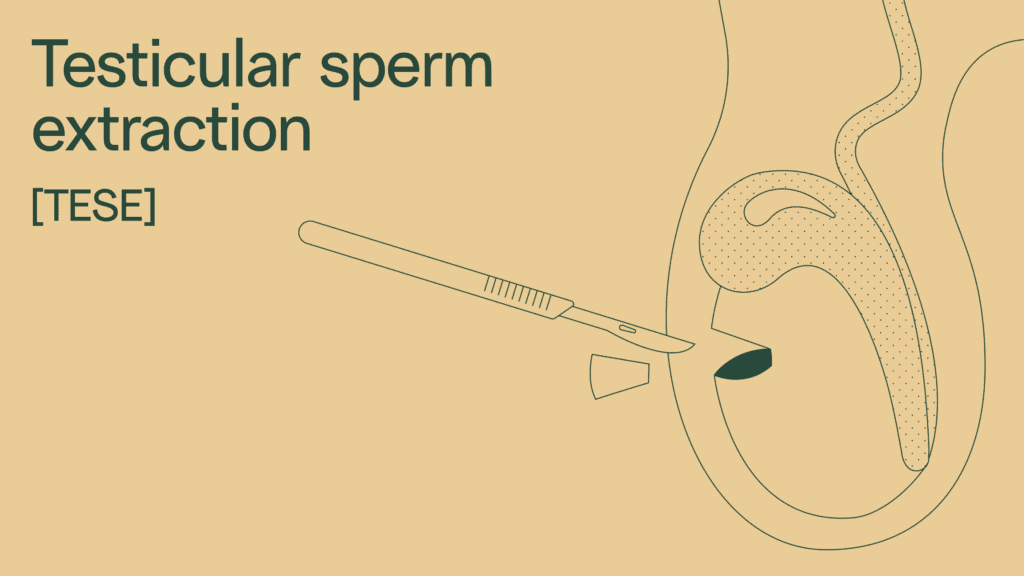
Testicular sperm extraction (TESE)
One of the most common sperm retrieval procedures is testicular sperm extraction (TESE). TESE is recommended for people with little or no sperm in their semen, known as obstructive azoospermia.
Lack of sperm might be caused by:
- Genetic conditions, like Klinefelter syndrome or Kallman syndrome
- An undescended testicle
- Vasectomy
Process of testicular sperm extraction (TESE)
Testicular sperm extraction (TESE) is a short procedure, usually around 20–45 minutes. It may use local anesthesia, sedation, or general anesthesia.
Using a scalpel, a doctor makes a small incision in the scrotum. The doctor will take a biopsy of testicular tissue and examine it under a microscope. If sperm is found, it can be frozen or used fresh in fertility treatments like IVF with ICSI. Testicular sperm extraction procedures help boost your chances of conceiving.
Microdissection TESE (microTESE)
In recent years, the more effective — yet more invasive — microdissection testicular sperm extraction (TESE) has led it to become the preferred option for many doctors. MicroTESE uses a microscope to more accurately identify testicular tissue that may contain sperm. According to the University of Utah, sperm is successfully found through microTESE procedures 60% of the time.
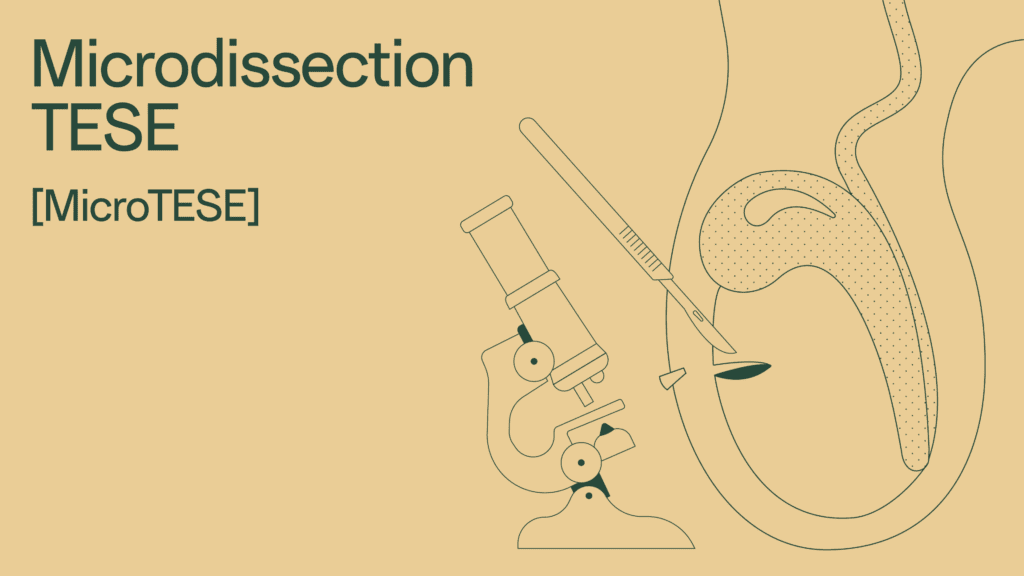
Process of microdissection TESE (microTESE)
Like traditional testicular sperm extraction, the patient is placed under general anesthesia and a small incision is made to open the scrotum. Unlike traditional testicular sperm extraction, the surgeon then uses a high-powered microscope to look for swollen seminiferous tubules. Think of these as the factory where sperm production takes place.
Because the doctor can be more certain sperm might be present, they can extract a smaller amount of tissue to be biopsied. MicroTESE may also eliminate the need to do multiple testicular sperm extraction procedures.
Testicular sperm aspiration (TESA)
Testicular sperm aspiration (TESA) is another common method for retrieving sperm. Instead of a scalpel, testicular sperm aspiration uses a needle and syringe to extract sperm from the testicle.
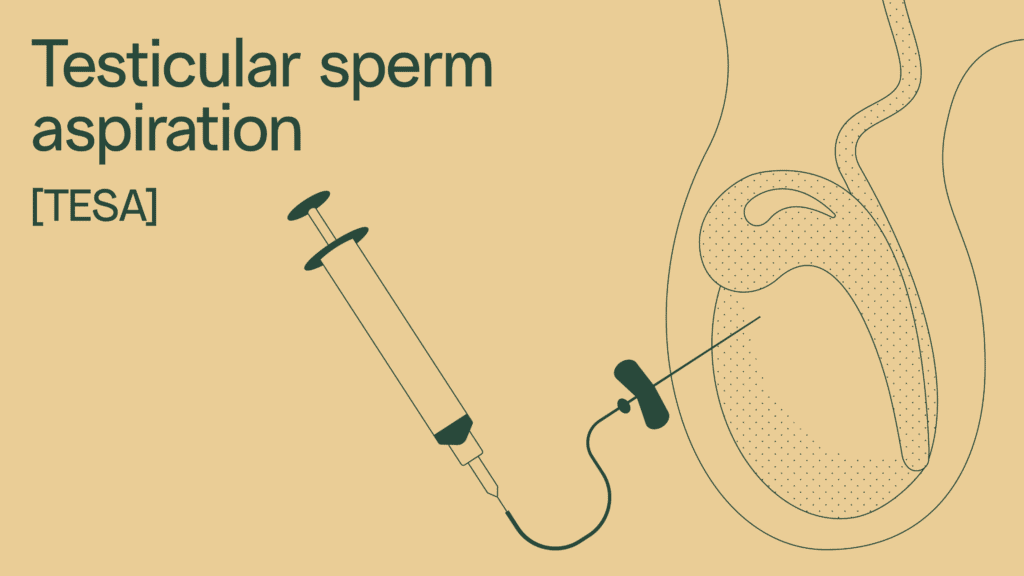
Though simpler and less invasive than testicular sperm extraction (TESE), it may not be as effective. In one study, patients who underwent testicular sperm aspiration (TESA) saw significantly lower sperm retrieval rates than testicular sperm extraction (TESE), as well as a lower presence of motile sperm (sperm that can “swim”).
Testicular sperm aspiration (TESA) is recommended for people with conditions that limit the amount of sperm in their semen, such as:
- Testicular blockages
- Genetic conditions or abnormalities
- Ejaculatory dysfunction
- Vasectomy
Testicular sperm aspiration (TESA) may also be used as a way for cancer patients to freeze their sperm before chemo or radiation.
Process of testicular sperm aspiration (TESA)
Testicular sperm aspiration (TESA) typically takes place under local anesthesia. During the procedure, a needle is inserted into the testicle to extract tissue and sperm cells. Often, this is repeated a few times in different areas. Once the sperm is examined and isolated, it can be frozen or used immediately in IVF with ICSI.
Micro epididymal sperm aspiration (MESA)
Micro epididymal sperm aspiration (MESA) is the preferred method of testicular sperm retrieval for congenital absence of the vas deferens. It’s also sometimes used for people who have had a vasectomy or have a blockage with inflammation or infection.
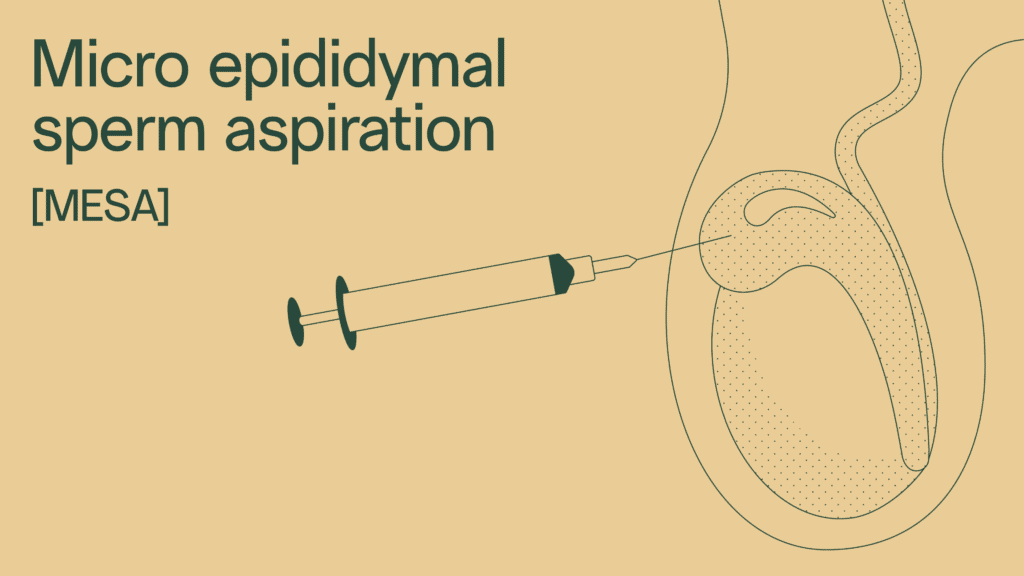
Process of micro epididymal sperm aspiration (MESA)
Under general anesthesia, an incision is made on the scrotum to expose the epididymis, the coiled tube behind each testis that stores sperm. The surgeon uses a high-powered microscope to identify sperm within the epididymal tubules. Using a very small blade, the tubes are opened, and the surgeon uses a syringe to collect the fluid inside the tubes.
Viable sperm found under a microscope can then be frozen and used in IVF or ICSI procedures.
Percutaneous epididymal sperm aspiration (PESA)
Percutaneous epididymal sperm aspiration (PESA) is the least invasive sperm retrieval option. It uses a needle like the one used to draw blood at a lab.
While not always as effective as other methods, PESA is often less expensive and less painful. Because it doesn’t require an incision, PESA can be repeated multiple times in one sitting — up to three times on the same epididymal tubule, according to one study.
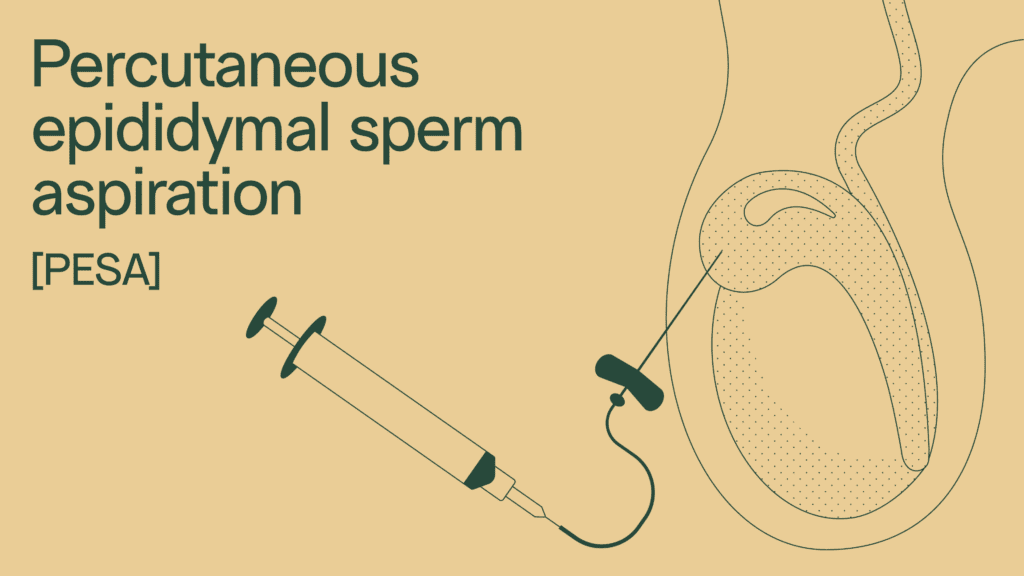
Process of percutaneous epididymal sperm aspiration (PESA)
Percutaneous epididymal sperm aspiration (PESA) begins with local anesthetic. A small butterfly needle is inserted into the epididymis and pressure is applied to the testicle until fluid flows through the tube. To make sure there’s enough sample to examine, the process may be repeated a few more times.
| TESE | MicroTESE | TESA | MESA | PESA | |
| Anesthesia | General or local | General | Local | General | Local |
| Surgical incision required | Yes | Yes | No | Yes | No |
| Source of sperm sample | Extraction of testicular tissue | Extraction of testicular tissue | Aspiration of testes | Incision and aspiration of fluid from the epididymis | Aspiration of fluid from the epididymis |
How to use sperm retrieved from the testes
The sperm that results from testicular sperm extraction can be used in IVF/ICSI procedures.
- In-vitro fertilization (IVF) is a method of assisted reproduction in which an egg is combined with sperm outside the body. The fertilized egg is then allowed to develop into a blastocyst embryo in the lab, before transferring it to a patient’s uterus to attempt pregnancy.
- Intracytoplasmic sperm injection (ICSI) is an in vitro fertilization procedure in which a single sperm cell is injected directly into the cytoplasm of the egg to accomplish fertilization.
Because testicular sperm extraction typically yields a low number of sperm, ICSI is usually the preferred method, and has a higher success rate for sperm retrieved from testicular sperm extraction (TESE), MESA, and other sperm retrieval techniques.
Diagnosing male-factor infertility
As you can see, how infertility is diagnosed and treated isn’t always black and white. If you’re struggling to conceive and considering IVF or ICSI, it might be a good idea to chat with your urologist about testicular sperm retrieval.
For most people, semen analysis is the first step. With results in 24 hours, Legacy’s sperm testing and freezing kit can get you an in-depth look at:
- The amount of sperm in your semen (sperm concentration)
- How active your sperm are (sperm motility)
- The total sperm count in your sample
Learn more about how at-home sperm testing works.