Testosterone replacement therapy, or TRT, is a prescription treatment for low testosterone. Read on to find out more about TRT, how testosterone replacement therapy works, and its risks and benefits.
A note on the focus of this article: Testosterone therapy is also administered to transgender men as part of gender transition (typically known as gender-affirming hormone therapy or GAHT). In this article, we’re discussing the treatment for cisgender men with symptoms of low testosterone, known as TRT.
Key takeaways
- What is testosterone replacement therapy (TRT)? It’s a therapy to treat low testosterone in men.
- Several forms of TRT are commonly prescribed. TRT methods include injections, topical gels, and implants.
- Is TRT safe? Testosterone therapy is FDA-approved for use in certain diagnoses, and can reduce the symptoms of low testosterone. However, TRT has side effects of its own, including infertility and increased risk of blood clots.
- TRT shuts down sperm production. If you’re considering TRT but might want kids in the future, freeze your sperm before you start.
What does testosterone replacement therapy do?
Testosterone is a sex hormone that’s essential for the body. Testosterone is responsible for sperm production, sex drive, secondary male sexual characteristics (like body hair and muscle growth), bone strength, and body fat percentage.
Testosterone levels decline with age, falling about 1–2% per year.1 After the age of 45, over 1 in 3 men have low testosterone. That number rises to 50% of men over age 80.2
Low testosterone can cause a number of symptoms, including:
- fatigue
- a decline in sex drive
- erectile dysfunction
- weight gain
- loss of body hair or muscle mass
- osteoporosis
- mood disorders such as anxiety or depression
Learn more about warning signs for low testosterone.
TRT increases the amount of testosterone in a man’s blood using a synthetic form of the hormone that was manufactured in a lab. The aim is to alleviate the symptoms that a low testosterone level may cause.
How is low testosterone diagnosed?
Testosterone is measured by a simple blood draw, done between 8am and 10am. (Fun fact: Testosterone is highest in the morning and lowest around 9pm.) There are two commonly measured “types” of testosterone:
- Free testosterone, or the amount of testosterone circulating in the blood. In most men, this represents 2% to 3% of their overall testosterone.
- Total testosterone, which includes free testosterone and testosterone attached to proteins in the body like sex hormone binding globulin (SHBG).
How is a “normal” testosterone level calculated? That can vary, depending on the healthcare provider and the lab they use. Low testosterone may be determined by looking at free testosterone, total testosterone, or a formula that considers the proteins testosterone binds to, including SHBG and albumin.
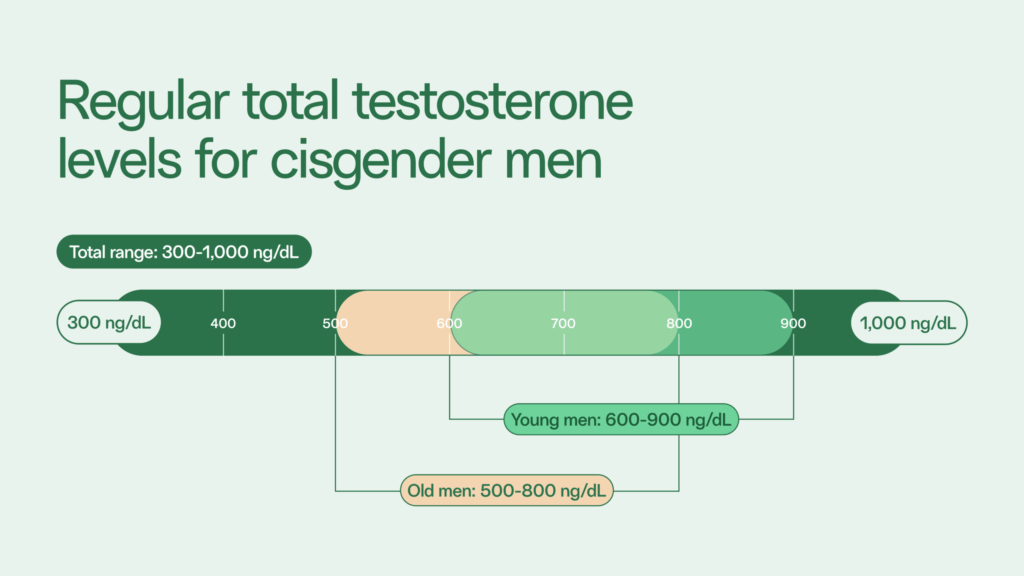
The normal range for total early morning testosterone is between 300 ng/dL to 1000 ng/dL.3 Low testosterone is generally diagnosed when that level is less than 300 ng/dL. Young adults should have a testosterone level between 600 and 900 ng/dL, while in senior men, a healthy level is considered between 500 and 800 ng/dL.4
Who might benefit from TRT?
If you’re experiencing those symptoms, your healthcare provider may suggest getting your testosterone level checked. It’s recommended you do this in the morning, when T levels are highest. An official diagnosis of low testosterone is generally made after two morning tests indicate low T. Then TRT may be prescribed.
Forms of TRT
Prescription TRT comes in various forms, including:
- Testosterone injection: An injection of testosterone into the muscle done every two to three weeks or every few months, depending on the prescription. They can be done in a doctor’s office or at home.
- Testosterone patch. A patch applied to the daily continuously delivers testosterone for 24 hours.
- Testosterone gel. Usually containing 1% testosterone, this is applied daily to the shoulders, stomach, or upper arm.
- Testosterone implant. Testosterone pellets may be implanted under the skin of the stomach or in the buttock muscle. They last for four to seven months.
- Nasal gel. This newer form of TRT comes as a gel applied to the nostrils. It needs to be used three times per day.
- Oral tablet or capsule. In February 2020, the FDA approved oral testosterone undecanoate for TRT. Previous oral forms of testosterone, such as methyltestosterone, were associated with liver injury, making healthcare providers reluctant to prescribe them.
What to expect when you start TRT
The typical TRT prescription lasts six months.5
Getting started on TRT should involve a discussion with your healthcare provider about the form of TRT that’s best for you, the dose, and potential side effects — including the potential impact on your sperm production.
As with any medication, your TRT dose may need to be adjusted. Some men like using the gel form of TRT for this reason; it’s easiest to apply more or less. Others do well with the “set it and forget it” aspect of testosterone implants.
Most symptoms of low testosterone can be resolved within a few weeks on TRT. Learn more about what to expect when you start testosterone replacement therapy.
What are the side effects of TRT?
Side effects of testosterone therapy treatment can include:
- Acne
- Sleep apnea
- Breast swelling or tenderness
- Swelling in the ankles
- An increase in red blood cells, and associated increased risk of blood clots
- Infertility
Does TRT cause cancer? TRT is not associated with a higher risk of prostate cancer. However, TRT can stimulate the growth of prostate cancer cells. For that reason, healthcare providers may not advise TRT if you’re at increased risk of prostate cancer.6
Does TRT cause hair loss? Studies suggest that TRT doesn’t directly cause hair loss. But increasing the level of testosterone in your body can increase the level of DHT, the hormone that causes hair loss if your hair follicles have a genetic sensitivity to it.
TRT and your sperm
One of the most significant — though often misunderstood — side effects of TRT is infertility. When the brain senses an external source of testosterone is being introduced to the body, it sends signals to the pituitary gland to slow or stop natural hormone production. This is known as a negative feedback loop.
Turning off the natural “tap” of male fertility hormones will reduce or stop sperm production, also known as spermatogenesis. For that reason, the majority of men who take TRT will be infertile within a few months.
Stopping TRT may allow sperm production to restart. However, it may not happen quickly — about 1 in 3 men on TRT don’t recover sperm production within 1 year. And it’s not guaranteed. In 10% of men who go on TRT, sperm production may never resume.5
Read more about testosterone therapy and fertility.

The National Institutes of Health says it plainly: “Testosterone should not be used for men seeking to produce a pregnancy as it significantly decreases sperm production.” If you’re considering TRT and still want biological children someday, you may want to consider freezing your sperm. It’s an easy insurance plan.
Read more about freezing sperm before TRT.
References
- 1. Stanworth, 2008. “Testosterone for the aging male; current evidence and recommended practice.”
- 2. Dandona et al, 2010. “A practical guide to male hypogonadism in the primary care setting.”
- 3. Anaisse et al, 2017. “Testosterone deficiency in adults and corresponding treatment patterns across the globe.”
- 4. Vermulen, 2002. “Diagnosis of hypogonadism in the aging male.”
- 5. Sizar et al, 2023. “Androgen Replacement.”
- 6. Harvard Health Publishing, 2023. “Testosterone: What it is and how it affects your health.”



