Guide to Sperm
Quality
Fertility is something that many of us will take for granted: have sex, get pregnant. However, it’s not always so straightforward. Infertility is a growing problem worldwide, affecting 1 out of every 7 couples. Male-factor infertility is estimated to cause about 1 in every 3 cases. Although infertility can be due to a variety of conditions, sperm quality is one of the most important predictors of fertility.
Let’s learn more about sperm quality, including sperm morphology, motility, and DNA fragmentation, as well as what might affect your sperm quality, and how to improve sperm health.

What is sperm quality?
Sperm quality refers to sperm’s ability to accomplish fertilization. Fertilization is impacted by several interconnected factors: sperm motility and sperm morphology, as well as by the health of the DNA carried by the sperm.
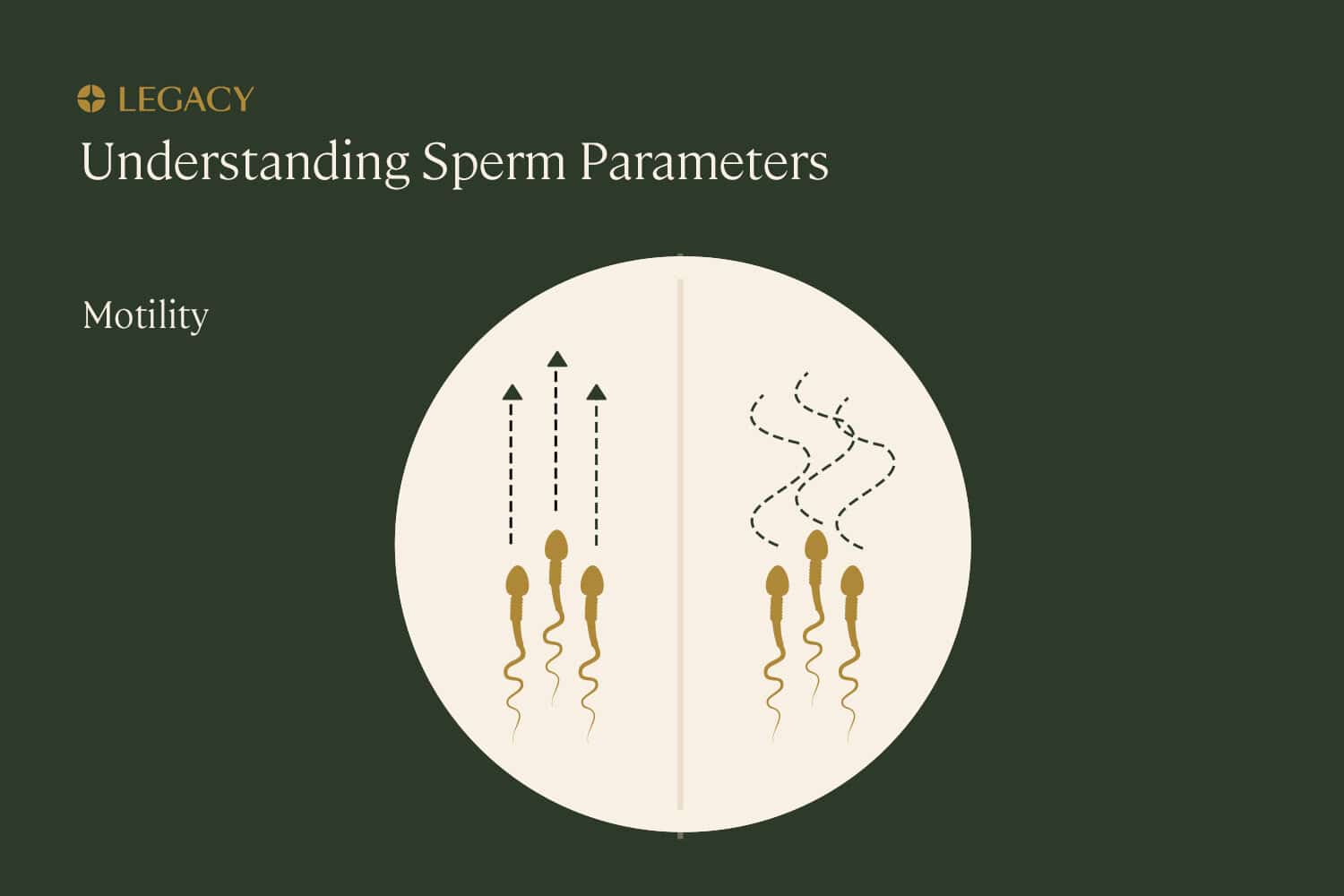
Sperm motility
Motility refers to the ability of the sperm to move or “swim,” which is essential for them to move through the female reproductive system and fertilize the egg.
Progressive motility is the best type of movement that can be seen in sperm quality testing. This means the sperm are moving forward in straight lines or in large circles, as opposed to in small tight circles or along erratic paths. Progressive sperm motility plays an integral role in sperm quality.
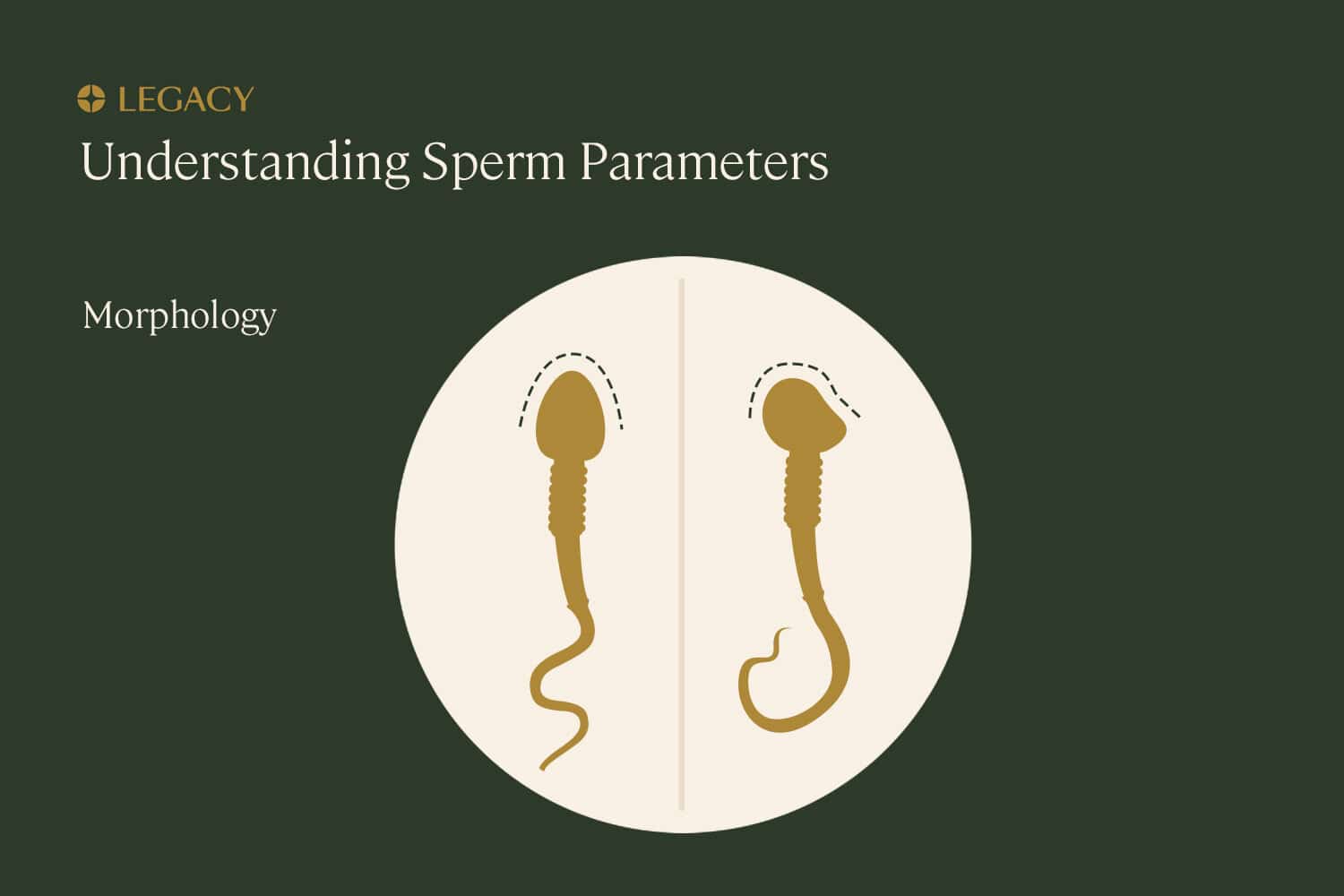
Sperm morphology
Morphology, another crucial factor for sperm quality, means the sperm’s structure or shape. Proper morphology includes:
- the sperm tail, made of protein fibers, which helps it “swim” toward the egg.
- the sperm midpiece, or body, which contains mitochondria to power the sperm’s movement.
- the sperm head, which houses the nucleus where the sperm’s precious cargo — genetic information — is stored. The head also includes the acrosomal vesicle, a tiny structure at the tip of the sperm full of enzymes that help the sperm penetrate the egg by digesting proteins and sugars on the surface of the egg.
This structure is important because it impacts a sperm’s ability to travel to, penetrate, and fertilize an egg.
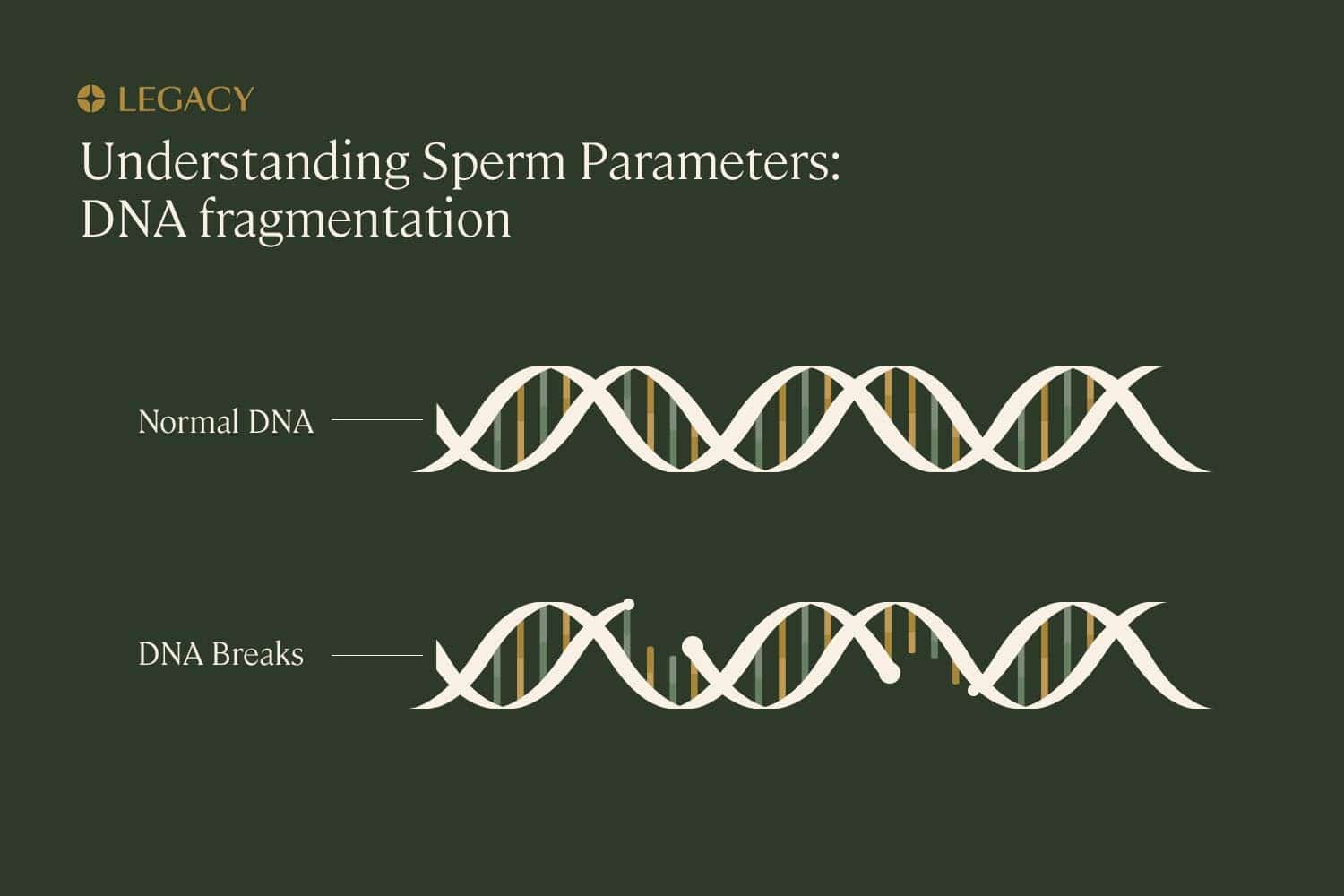
DNA health (fragmentation)
Each sperm cell should contain 23 chromosomes. Chromosomes are molecules of DNA, the material that guides the growth and development of the entire human body.
Sperm cells are known as “haploid” cells, meaning they contain half the number of chromosomes in a typical human cell. The egg contains the other half. Together, they create a fully realized cell of 46 chromosomes (known as a “diploid” cell), which then divides to become all of the other cells in the body.
As you might imagine, this means the integrity of genetic material carried by sperm is essential for successful fertilization and normal embryo development. Sometimes, the DNA inside sperm can become damaged, broken, or otherwise abnormal, known as sperm DNA fragmentation. DNA fragmentation directly correlates to lower fertility in men, and is also linked to recurrent pregnancy loss (two or more consecutive miscarriages).
DNA fragmentation can be caused by many factors, including age, fever/illness, smoking, and exposure to toxins. Learn more in our guide to sperm DNA fragmentation to understand how it can affect sperm quality.
Sperm quality vs. quantity
The other half of the sperm equation is sperm quantity, or sperm count/concentration. Sperm concentration refers to how densely packed those sperm are within the semen. Sperm count is the total number of sperm in a particular quantity of semen, the fluid that carries sperm out of the penis. For example, a sample may include 3 milliliters of semen with a sperm concentration of 15 million sperm per mL; that would add up to a total sperm count of 45 million.
Sperm quantity and sperm quality are separate factors. A high sperm count isn’t entirely helpful to fertility if most of those sperm are misshapen, can’t swim properly, or carry damaged DNA. But sperm quality issues and low sperm count can be caused by some of the same things, including exposure to toxins or chemotherapy, smoking, and hormone imbalance.
What affects sperm quality?
These are just a few of the most common factors affecting sperm quality:
Age and sperm quality
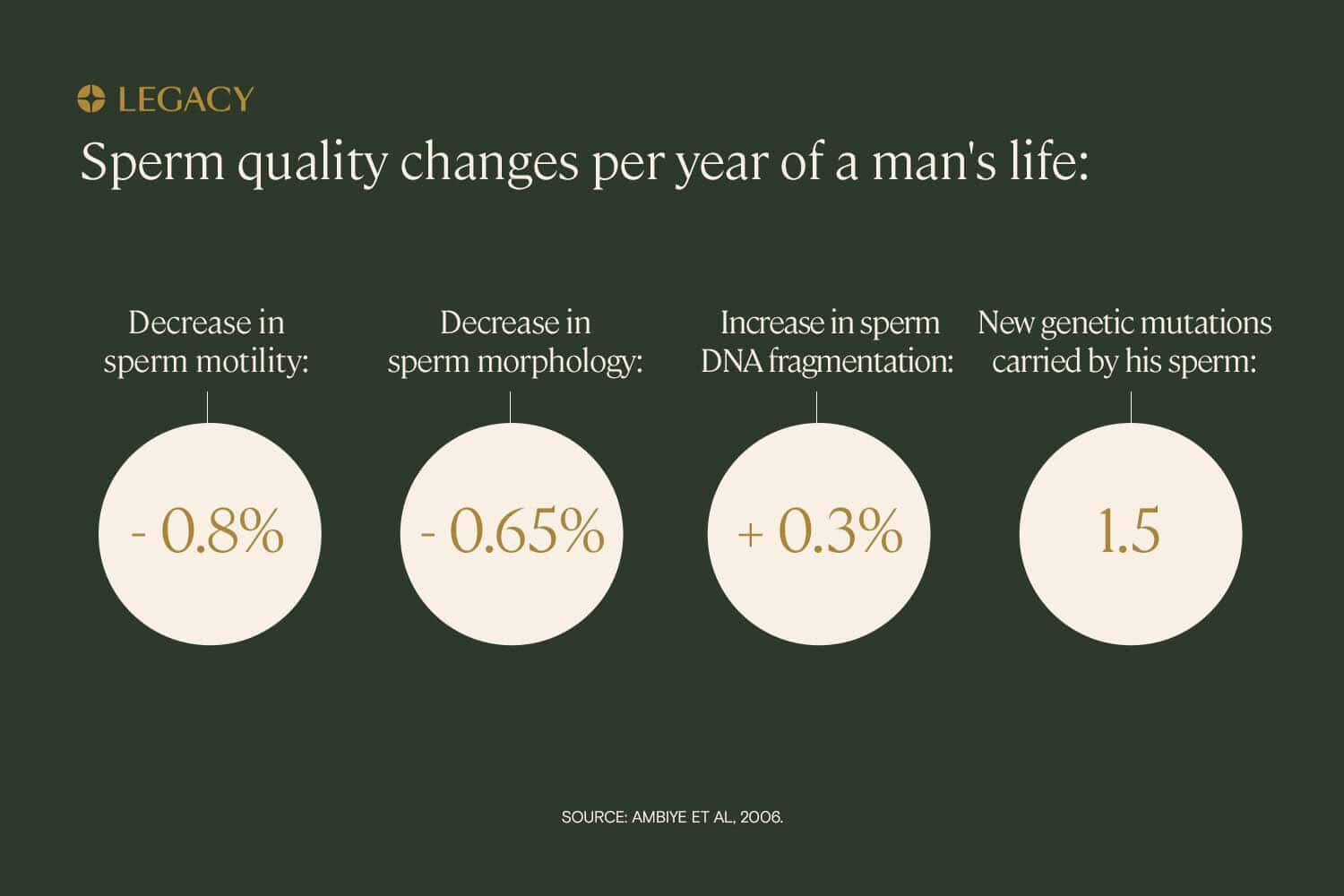
As a person ages, their sperm motility decreases. According to one study, sperm motility decreases, on average, about 0.8% per year. Additionally, they’ll have lower numbers of sperm with normal morphology. Research indicates that normal sperm morphology declines 0.2–0.9% per year, resulting in a 4–18% decrease in normal morphology over a 20-year period.
The sperm of older people is more likely to have higher rates of DNA fragmentation, as well as additional genetic mutations that can lead to schizophrenia, autism, and more. The best way to prevent the issues associated with aging sperm is to freeze your sperm at a younger age. Learn more about sperm freezing options.
Lifestyle factors and sperm quality
The good news? Your body is making sperm constantly. So if you make a lifestyle change for the better, you could see sperm quality improvements in as little as 2–3 months. Learn more in our guide to sperm quality improvement.
Medical history and sperm quality
Certain medications, such as testosterone replacement therapy, anabolic steroids, antidepressants, chemotherapy drugs, opiates, and NSAIDs, may have an impact on sperm quality and sperm production. Whether this impact is reversible depends on the type of medication, dosage, and how long the drug is taken.
Additionally, a recent history of infection, illness, or fever can affect sperm quality. In most cases, the effect on sperm quality is temporary.
Toxin exposure and sperm quality
Certain chemicals are known to impact sperm quality:
- Lead
- Pesticides
- Hydrocarbons
- PCBs, the chemical compounds found inside transformers
- Cadmium
- Diesel exhaust
- Petrochemicals
- Solvents
- Many more
Exposure to these toxins is twice as prevalent among infertile men as it is among healthy men.
While the toxins in everyday household products may also be damaging, due to long-term contact, we’re typically most concerned about those who are exposed to toxins through their occupations. Those who work in agriculture and herbicides, plastic production, and the military have, on average, worsened sperm parameters and sperm quality.
Testing your sperm quality
Sperm count and sperm quality (morphology and motility) can be tested with a semen analysis.
This test involves providing a semen sample, collected via masturbation, to a lab. In the lab, it will be examined under a microscope to determine your sperm concentration, your sperm motility, and your ratio of properly formed sperm (sperm morphology).
The test can be done in a fertility clinic or urologist’s office, or can be done from the comfort and privacy of home with a mail-in sperm testing kit. The results of your semen analysis will tell you which of your sperm quality parameters are normal, and which (if any) are abnormal.
The Legacy semen analysis report also includes personalized recommendations for sperm quality improvement, based on your lifestyle, and tips for how to increase sperm morphology.
Learn more about sperm testing options and test your sperm quality.

DNA fragmentation testing
A typical semen analysis doesn’t test the genetic health of sperm. A more in-depth test is required to evaluate DNA fragmentation sperm. Legacy offers the first and only easy at-home sperm DNA fragmentation analysis.
How to improve sperm morphology, motility, and genetic health

Start an exercise regimen for sperm quality
Simple, low-intensity workouts (such as walking, biking, or jogging) have a considerable benefit for sperm quantity and sperm quality. Learn more about exercise and sperm health and physical activity’s impact on sperm quality improvement.

Improve your diet to improve sperm quality
What you eat can affect sperm quality. The best diet for sperm quality improvement is a balanced, Mediterranean-style diet rich in:
- Fruits
- Vegetables, especially leafy greens
- Fish and other seafood
- Nuts and seeds
- Healthy fats
Moderate in:
- Soy products
- Lean protein
- Caffeine
And low in:
- Added sugars
- Processed meats
- Trans fats

Quit smoking and reduce drinking
Having more than 5–7 drinks per week may dampen testosterone production, and negatively affects all aspects of your sperm quality including sperm count, concentration, and morphology.
Smoking can be especially bad for sperm morphology, creating genetic defects that lower sperm quality. Learn more about smoking and sperm health and how tobacco impacts sperm quality.

Get enough sleep to support sperm quality
Chronic sleep deprivation (regularly getting less than 6–7 hours a night) may reduce testosterone levels, lower sperm count and motility, and increase levels of anti-sperm antibodies, further damaging your sperm and lowering sperm quality. Learn more about sleep and male fertility.

Avoid certain drugs
Examples include testosterone, anabolic steroids, SSRIs, chemotherapy drugs, opiates, NSAIDs, and any other medication that has an impact on sperm quality.

Boost your diet with sperm quality supplements
Many supplements are associated with sperm quality improvements and increased sperm count and testosterone production. Learn more about male fertility supplements and sperm quality supplements.
After making lifestyle changes, you’ll want to retest with another semen analysis to see if your efforts have led to sperm quality improvement. Remember that the process of making sperm takes around 74 days, so you’ll want to keep up your new habits for 2–3 months before retesting for sperm quality.
Further reading: Legacy’s Guide to Sperm Improvement.
References
- E. Sloter et al. “Quantitative effects of male age on sperm motion.” Human Reproduction, 2006.
- L. Bujan et al. “Sperm morphology in fertile men and its age related variation.” Andrologia, 1988.
- Victor Pino et al. “The effects of aging on semen parameters and sperm DNA fragmentation.” JBRA Assisted Reproduction, 2020.
- Pravesh Kumar Bundhun et al. “Tobacco smoking and semen quality in infertile males: a systematic review and meta-analysis.” BMC Public Health, 2019.
- Jaime Mendiola et al. “Exposure to environmental toxins in males seeking infertility treatment: a case-controlled study.” Reproductive BioMedicine Online, 2008.
- Paul Claman, MD. “Men at Risk: Occupation and Male Infertility.” Sexuality, Reproduction & Menopause, 2004.