Guide to Sperm Freezing
If you’ve ever considered sperm cryopreservation, commonly known as sperm freezing or sperm storage, you probably have a lot of questions about how it works, what to expect, how effective sperm freezing will be for you, and when you should turn to sperm freezing.
Our Guide to Sperm Freezing will break down everything you need to know about sperm freezing — from why people consider sperm freezing to longevity, sperm freezing costs, sperm storage options, and more.
Table of contents

What is sperm freezing?
Sperm freezing, also known as sperm cryopreservation, is the process of using liquid nitrogen to freeze one or more sperm samples for possible use later on, when healthy sperm may be harder to acquire. Sperm freezing essentially preserves your option to become a biological parent, regardless of age, illness, injury, medical treatment, or life path.
Who should consider sperm
freezing?
The first successful pregnancy with frozen sperm was recorded in 1953 and, since then, sperm freezing has been a recommendation for male cancer patients before undergoing radiation therapy treatment.
That isn’t the only reason for sperm freezing, though. There are many other factors that make sperm cryogenic storage a proactive choice. While this isn’t an exhaustive list, here are some of the more common reasons that people may consider sperm freezing and sperm storage.
Sperm freezing for cancer
patients
The LIVESTRONG organization estimates that, in up to 75% of cancer patients, fertility may be impaired as a result of cancer treatment. These are life-saving treatments, and infertility is not a reason not to proceed. But as cancer therapies and survival rates improve, we can thankfully focus on the quality of life of cancer survivors, and that includes their ability to have a family if and when they want.
Some cancer treatments, including chemotherapy, hormone therapy, radiation therapy, surgery, and bone marrow transplants, carry a risk of negatively impacting male fertility. In some cases, these treatments can cause irreversible damage.
For example, radiation therapy has been shown to cause gonadal damage, resulting in azoospermia (the inability to produce sperm) in patients. Similarly, chemotherapy has been shown to impact the Sertoli and Leydig cells, which are both essential to the process of spermatogenesis (sperm production).
Cryopreservation and sperm storage have provided a safe and effective means for having children in the future. Among the many questions and conversations you’ll have with your doctor before undergoing any form of cancer treatment, fertility preservation may be one of those conversations to be had.
Sperm freezing for trans women
Sperm-producing transgender individuals may want to have biological children in the future, using their sperm to fertilize either a partner’s egg or a donated egg. Sperm freezing makes this possible, and is recommended before undergoing gender-affirming hormone therapy (typically estrogen and androgen-blockers).
A 2017 review looked at nearly 40 years of research on the impact of cross-sex hormones on the sperm quality and testicular function of trans women. The review found that, in the majority of cases, estrogen and/or anti-androgen treatment caused reduced or halted spermatogenesis, as well as physical changes to the testicles.
The effect seems to be dose-dependent; in one study, a low-dose estrogen therapy had no impact on sperm concentration or motility, while a higher-dose regimen resulted in reduced sperm motility after a few days and reduced sperm concentration after 2 weeks.
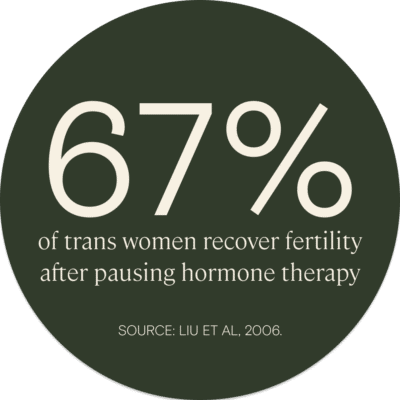
In some cases, sperm count and quality can be recovered. One study suggested that, within 6 months of stopping estrogen therapy, 67% of subjects returned to a normal sperm count.
However, the impact of medical gender transition on fertility, as well as the capacity for spermatogenesis to recover if estrogen treatment is paused, seem to be variable and individual. Case studies demonstrate that, while some patients continued spermatogenesis through gender-affirming hormone treatment, others stopped producing sperm altogether, and several experienced azoospermia for 4–5 months after pausing therapy.
Sperm freezing prior to hormone therapy offers an option for trans women to preserve their ability to become a genetic parent, and to avoid the need for long-term cessation of their hormone treatment later on.
Historically, many trans people did not get adequate counseling on their fertility prior to starting hormone therapy. That seems to be changing. A study in 2018 analyzed sperm samples in a sperm bank, finding that the number of transgender sperm bankers increased by 18% relative to cisgender sperm bankers from 2006 to 2016.
Those considering a vasectomy
A vasectomy is a highly effective contraceptive option. During a vasectomy, the vas deferens — the tube that brings sperm from the testes to the penis — is cut and sealed.
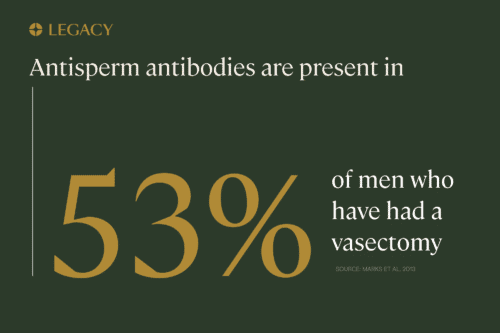
According to research, approximately 3–6% of vasectomy patients (or possibly even 10%, according to some estimates) change their minds and opt for reversal surgery. This may be due to a new marriage, the death of a child, change in financial situation, or a couple simply changing their mind and deciding they want children.
Sperm freezing: a better option than vasectomy reversal
Although vasectomy reversal surgery is an option, the success rate isn’t guaranteed. Dr. Honing of Yale Medicine says that success rates are 80–90% when performed by an experienced microsurgeon. However, some estimates of pregnancy rates after vasectomy reversal are as low as 30%.
The procedure can take 3–4 hours, substantially longer than the typical 15-minute vasectomy, because reversals are technically challenging surgeries. During a vasectomy, the vas deferens, which is the tube that stores sperm and carries it out of the scrotal sac, is severed. Those severed ends have to be reconnected with a great deal of precision during a vasectomy reversal to allow the sperm to once again enter ejaculate.
Research says that factors such as your surgeon’s skill level, secondary obstruction in the epididymis, or scar tissue in the vas deferens can contribute to ineffective vasectomy reversal.
Sperm freezing is significantly less expensive and invasive than attempting vasectomy reversal. Sperm freezing and sperm storage before a vasectomy provides you with a back-up plan, just in case you change your mind. With this option, you can choose to have another biological child without having to undergo vasectomy reversal surgery.
Members of the military
Military service is a high-risk career. There is the possibility of combat-related injury and exposure to chemical warfare or toxins, both of which can negatively impact a male’s fertility or a couple’s pregnancy outcomes.
A study of veterans of the US War on Terror found that rates of infertility were significantly higher — nearly twice as high — among veterans compared to civilians. Male veterans reported an infertility rate of around 14%, while female veterans reported 16%; in the general population, the rates are about 7% and 9%, respectively.
An older study of Gulf War veterans in the early 1990s found a similar trend: vets were at a 40–50% higher risk of infertility and miscarriage.
An analysis of the generational health effects of serving in the Gulf War reported that paternal exposure to pesticides at work was associated with an increased risk of having a preterm birth, and that paternal exposure to other chemicals, heavy metals, or petroleum products at home or at work increased the risk of a child born with birth defects.
One study referenced in the book compared the semen parameters, fecundity, and follicle-stimulating hormone (FSH) levels were measured in 64 men exposed to chemical agents such as mustard gas to 64 veterans with injuries, but no sulfur mustard exposure. Male factor infertility was diagnosed in 22.6% of those exposed and 4.9% in unexposed subjects.
Understanding these potential risks, military personnel may choose to preserve their fertility through sperm freezing and sperm storage before deployment.
Learn more about sperm freezing for members of the military.
Those who work in high-risk environments
In addition to military service, there are a number of professions that pose an increased risk of male infertility. People in these occupations may consider sperm freezing and sperm storage to preserve their fertility early in their careers.
Research shows that sperm-producing people who work in following industries may see a negative impact on their fertility, including reduced sperm count and increased risk of miscarriage and birth defects:
- Agriculture
- Herbicides
- Construction
- Machining
- Plastic production
- Printing
- Tobacco processing
- Welding
The evidence points towards exposure to toxic substances, such as pesticides, lead, metals, petrochemicals, and more.
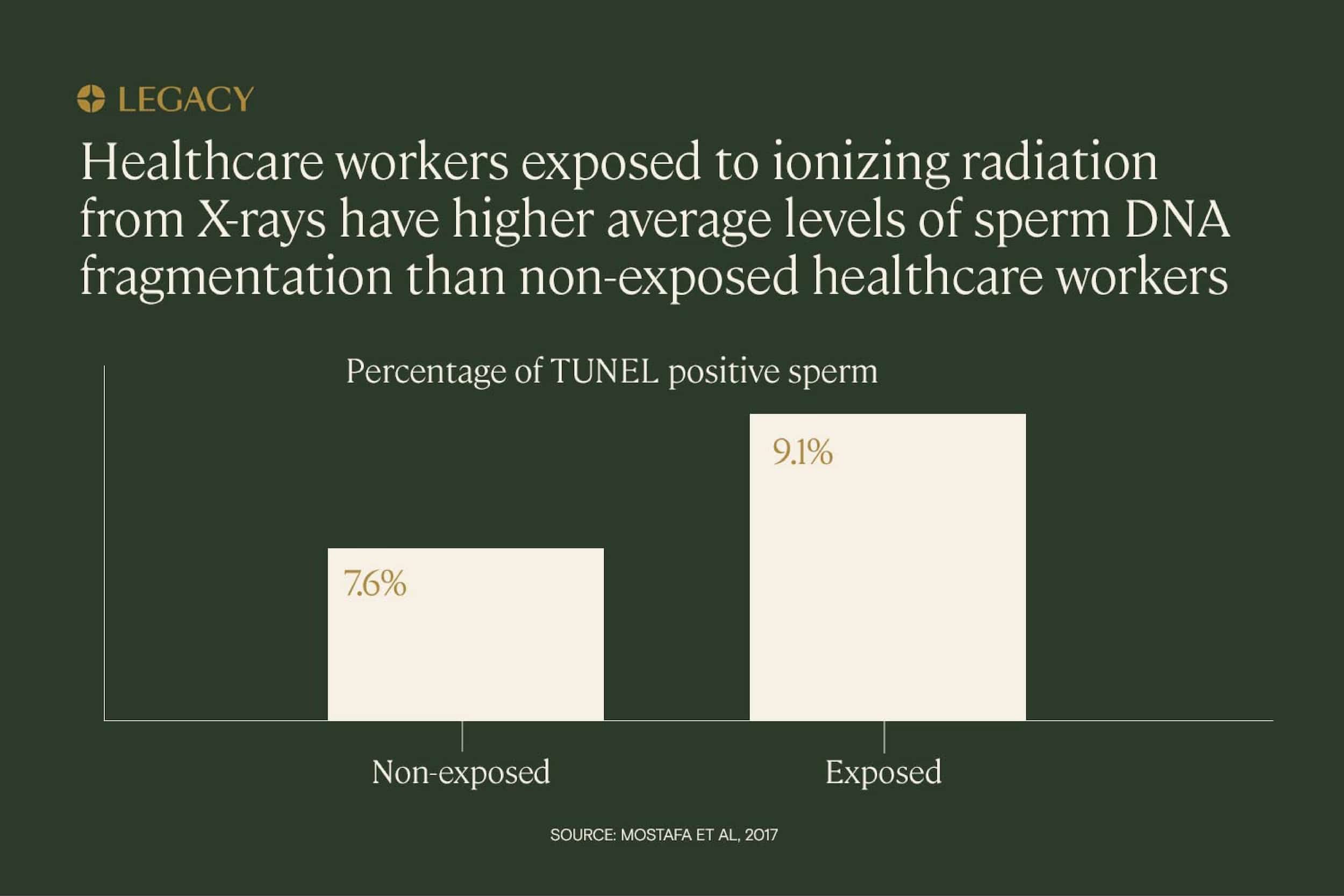
Exposure to radiation can also negatively impact male fertility. A study that analyzed 90 male radiographers against 90 men not exposed to x-ray radiation showed that there was significant association between exposure to radiation and miscarriage, congenital anomalies, still birth, and infertility.
Those who may have children later in life
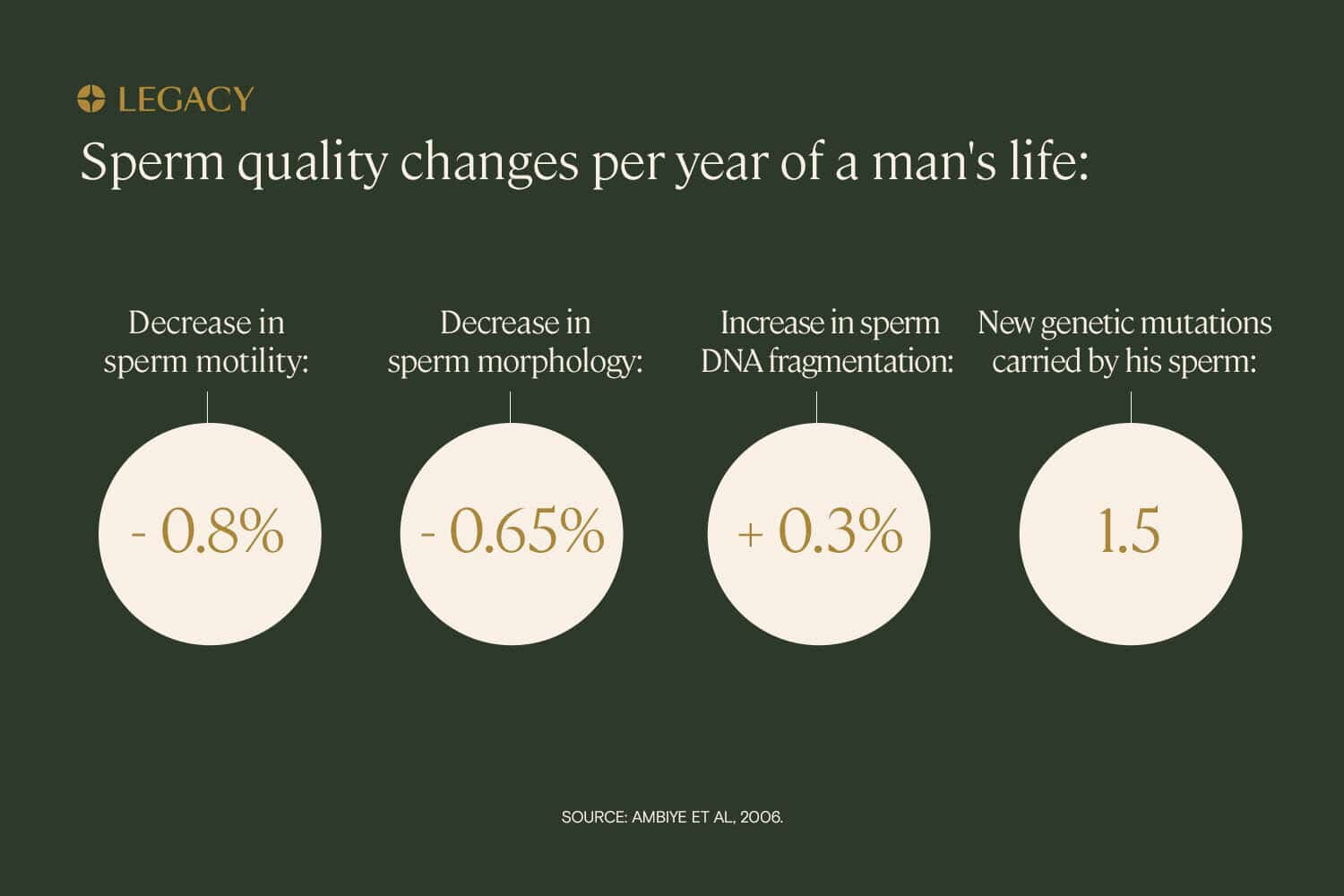
Although men have been known to father children well into their 60s and beyond, it is known that sperm quality decreases after the age of 35. This includes a significant decrease in pregnancy rate, an increase in time to conception, an increase in miscarriage risk, and an increase in potential adverse pregnancy outcomes.
All of this occurs because sperm quality parameters (count, motility, morphology, and DNA fragmentation) naturally change with age. On average, a male can expect to see a 0.8% decrease in sperm motility, 0.65% decrease in sperm morphology, and a 0.3% increase in sperm DNA fragmentation each year.
Sperm freezing in your 20s or 30s can help provide assurance for when you’re ready to have children later in life — especially if you don’t foresee starting a family until you reach your 40s.
Anyone who wants peace of mind about their fertility
Even when you do your best to plan for the future, sometimes life veers from your course. Freezing your sperm at its youngest and healthiest can help provide peace of mind that no matter what happens in the future, you have a plan B you can count on.
How the sperm freezing process works
Learn more about the sperm freezing process and how it works, including how to prepare for sperm freezing and how sperm is analyzed.
Sperm freezing
step 1: Preparation
There is some testing that should ideally be completed before sperm freezing. In general, you’ll want to ensure you’re freezing the healthiest possible sample.
Before sperm freezing, you should do a screening for sexually transmitted diseases and infections that can impact sperm quality. This is also to reduce transmission to partners during artificial insemination, and is required in many states if you may use your frozen sperm in in vitro fertilization (IVF) treatment.
Legacy includes STI testing with our sperm testing and freezing packages, and offers an STI test kit for all clients.
It is also recommended to get a sperm analysis, which will provide you with data on your semen volume, sperm count, sperm concentration, sperm motility, and sperm morphology. If your sperm quality parameters aren’t where you want them to be, you can begin implementing lifestyle changes that have been shown to improve sperm quality, such as diet and exercise. You might also have recommendations from your doctor or fertility expert to follow.
Learn more about sperm improvement.
Sperm freezing
step 2: Producing a sample
If you choose to visit a fertility clinic or sperm bank, you’ll likely have some paperwork to fill first. Then, you’ll produce your sample in a private collection room, by manual stimulation to ejaculation (masturbation).
Using an at-home sperm freezing kit
For some, the thought of having to schedule an appointment and produce a sample in a stark, clinical facility can feel off-putting. In these cases, at-home sperm analysis and at-home sperm freezing kits, like Legacy’s, provide another path.
With this method, you are mailed an at-home sperm freezing kit that provides you with a secure storage vessel to collect your sample at home. You’ll mix your sample with a transport media that will protect it during shipping. Then, you can schedule same-day pick-up for your sample to be mailed overnight.
Learn more about how Legacy works as well as our sperm freezing options with our at-home sperm freezing kits.

Sperm freezing step 3: Processing and analyzing sperm
After sperm is received by the lab, it’s measured to assess semen volume before being “washed” with a sterile media. The sample is then centrifuged (spun) to separate the sperm from the seminal fluid and transport media.
This process allows the lab technicians to see just the sperm under a high-powered microscope. Many labs, including ours, use CASA, or computer-assisted sperm analysis technology to ensure accurate and consistent measurements of the key semen parameters: sperm count, motility (how many sperm are moving), and morphology (how many sperm are properly shaped).
Learn more about sperm testing.
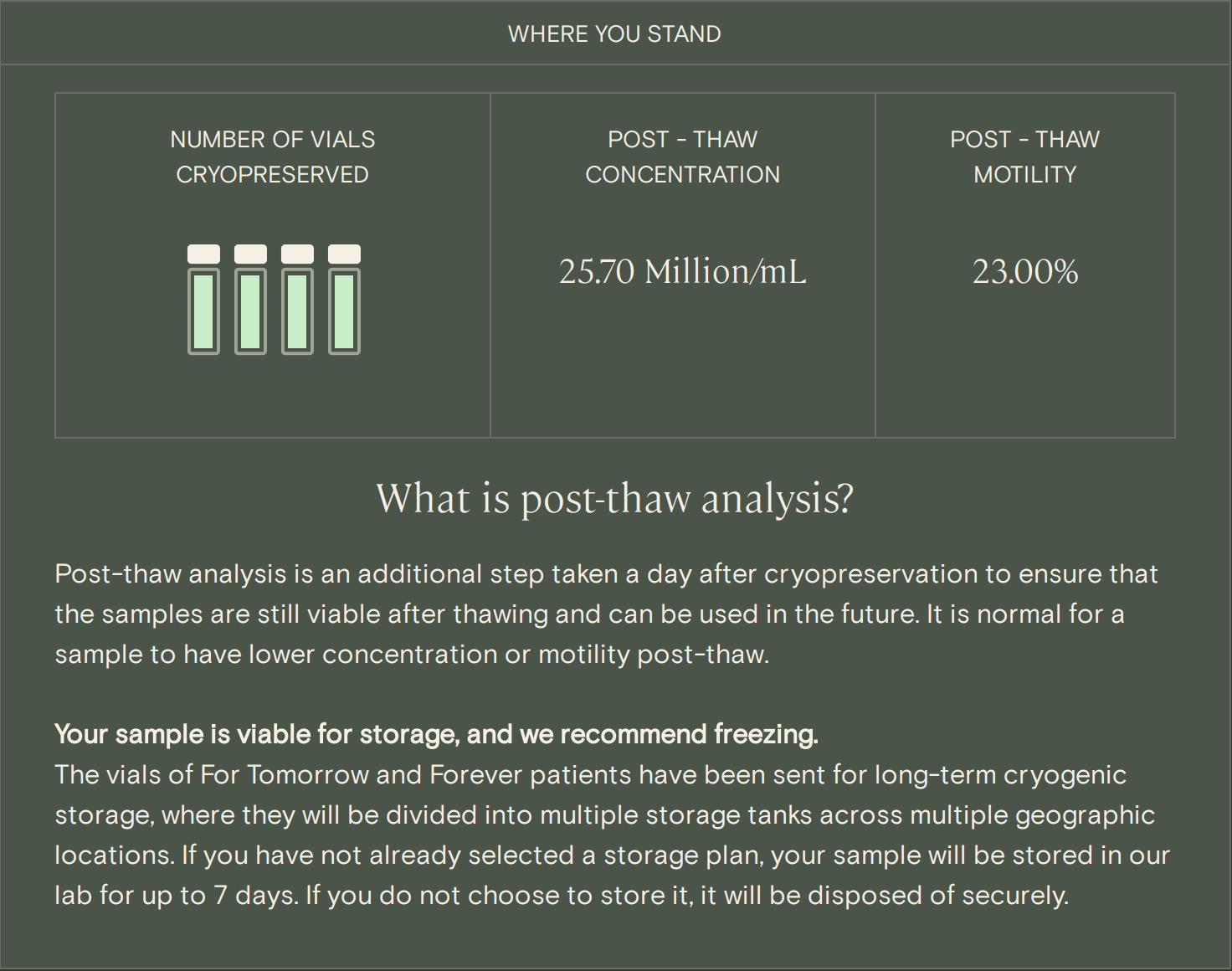
Sperm freezing step 4: Post-thaw analysis
This quality test is a critical step in sperm freezing and sperm storage. The post-thaw analysis involves freezing and then thawing a small portion of your sample, simulating the thawing conditions your sperm will experience in the future when it’s ready to be used. From there, we re-analyze sperm quality parameters to see if the sperm in your sample is viable after thawing.
According to research, it is normal to expect parameters like sperm motility to decrease a bit after being frozen and thawed. A recent study demonstrated that, on average, around 80% of sperm will survive the thaw.
This slight drop in numbers does not affect pregnancy rates significantly. For successful intrauterine insemination, data shows that around 10 million sperm is usually required. Those with normal, healthy sperm quality parameters usually produce at least 40 million sperm per ejaculate.
A post-thaw analysis gives you a realistic idea of the quantity and quality of sperm you may have after thawing, which is important information for the healthcare provider who may be working with the sample in the future.
A post-thaw analysis is conducted as part of every Legacy analysis, to determine whether or not a sample is eligible for cryostorage. In fact, Legacy offers the only at-home sperm freezing kit with a post-thaw analysis.
Sperm
freezing step 5: Cryopreservation and storage
How is sperm frozen? It’s a bit more complex than using a common home refrigerator.
Sperm is frozen using liquid nitrogen. First, sperm are gently mixed with a cryoprotectant, a substance that draws water out of the sperm cell to prevent damage during freezing, in cryogenic vials. Next, they are plunged into liquid nitrogen to freeze them at a temperature of -196ºC or lower.
Finally, the sperm vials are transferred to liquid nitrogen storage tanks to maintain their low temperature for long-term sperm storage.
How much sperm should I freeze?
The amount of sperm you should freeze depends on your family planning goals, your sperm count, and the quality of your sperm after it is thawed.
Each semen sample typically yields four vials of sperm. One vial of sperm equals one attempt at intrauterine insemination (IUI), which has a success rate of 10–20%. With IUI, it’s recommended that you freeze 3–5 vials per pregnancy you hope to have.
If you’re planning on using your frozen sperm samples for IVF with intracytoplasmic sperm injection (ICSI), a technique that involves injecting one sperm into the egg to fertilize it before transferring it into the uterus, you don’t need to freeze as much. With ICSI, a single vial of sperm can be used a nearly unlimited number of times, since there are typically hundreds of thousands (or millions) of sperm in one vial.
If you want to have a large family in the future, you will likely want to preserve more samples than someone is planning for one child. If your sperm count or quality is lower than anticipated after an analysis, it may also be recommended to preserve additional samples.
We recommend making multiple “deposits,” since sperm quality may be variable. Ideally, you would freeze multiple samples, and use your best sample when in the future.
How and where is frozen sperm stored?
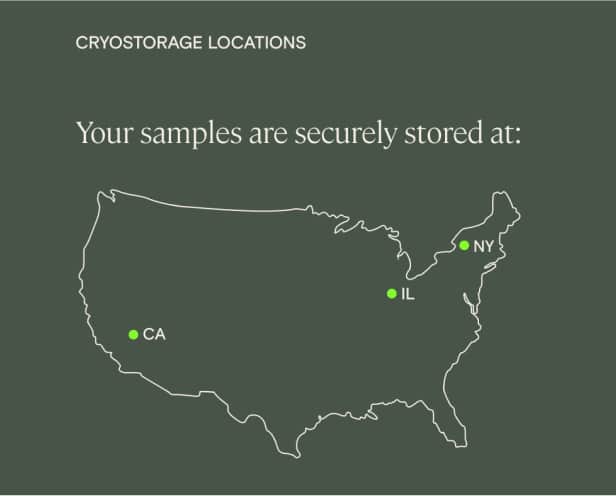
Frozen sperm is stored in cryogenic vials within liquid nitrogen or nitrogen vapor storage tanks, called dewars. The safest place for frozen sperm storage is a dedicated cryogenic storage facility, with security and ongoing monitoring of liquid nitrogen levels in the sperm storage tanks. That’s exactly where they’ll go after sperm freezing with Legacy.
Legacy frozen sperm safety measures
Legacy’s state-of-the-art cryogenic sperm storage facilities are monitored around the clock, with backup emergency power sources and equipment redundancy to mitigate the risk of a blackout or natural disaster.
To further mitigate any risk, Legacy offers multi-site frozen sperm storage as a default for all clients. That means your frozen sperm samples will be shipped to multiple cryo storage facilities, just in case.
Privacy and security measures
Cryo storage facilities are highly secure locations. For example, Legacy’s cryo storage partner facility employs a 24/7 video monitoring surveillance system along with motion detectors. Card-controlled access areas admit only trained and certified staff.
Cryostorage facilities must be HIPAA-compliant. HIPAA is a federal law that protects sensitive patient health information, so that means your samples cannot be released to anyone other than you or an individual that you have authorized (such as your spouse). Clinics and labs also cannot share your sample or storage details with third-parties, and must protect your health data and any associated personally identifiable data from unauthorized parties.

How long can your sperm stay frozen before using it?
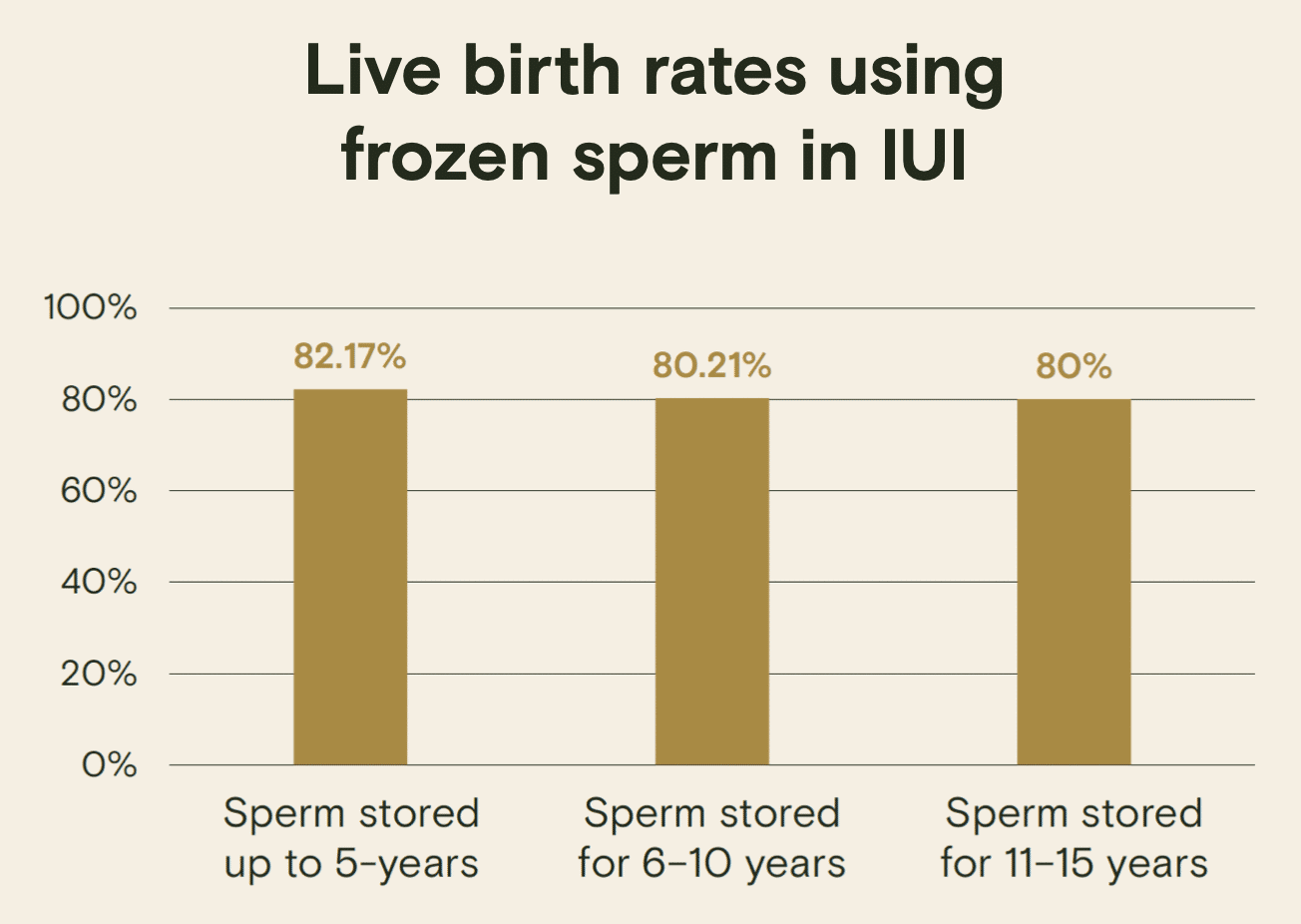
Essentially, sperm can last indefinitely when stored under the proper conditions.
A recent study examined the long-term effect of sperm freezing and found that there was no effect on sperm survival rate for the first 5 years of cryostorage. After 5 years, there was a small decrease in sperm survival rate, but this did not appear to significantly affect birth rates when the sperm was used in artificial insemination.
The study concluded that the length of cryostorage did not have a notable impact towards clinical outcomes.
Options for using frozen sperm
There are a number of options for using frozen sperm, including intrauterine insemination (IUI), in vitro fertilization, and IVF with intracytoplasmic sperm injection.

Intrauterine insemination (IUI)
During IUI, thawed and prepared sperm is inserted directly into the uterus, bypassing the vagina and cervix. The procedure happens at the time of ovulation, often timed using ovulation medication.
A 2022 study found that pregnancy rates using frozen sperm in IUI were similar to pregnancy rates using “fresh” sperm. Generally, if your total motile sperm count (TMSC) is more than 8 million, IUI is an option for you after sperm freezing.

In vitro fertilization (IVF)
IVF is a process in which eggs are retrieved from a patient’s ovaries surgically and fertilized with sperm in the lab. If a patient’s post-thaw motility is high enough, they will have the option to do IVF without ICSI.
Research shows that chances of pregnancy with IVF are no less with frozen-thawed than with fresh semen.

IVF with intracytoplasmic sperm injection (ICSI)
ICSI is an IVF technique in which a single sperm is injected directly into an egg. It’s most useful in cases of male-factor infertility, when sperm motility is low. Multiple studies (1,2) have shown that pregnancy rates are equivalent when using frozen sperm in IVF with ICSI, compared to fresh.
How much does it cost to freeze sperm?
When freezing sperm at a fertility clinic or sperm bank local to you, the cost of sperm freezing will vary significantly, depending on your region and the facility you choose. According to the LIVESTRONG, the initial testing and sperm freezing cost can total $1,000, with an additional $300–500 (or more) per year for ongoing sperm storage.
Unfortunately, most medical insurance in the US does not cover sperm preservation and sperm storage (except, sometimes, in the case that it’s necessary before cancer treatment or other medical treatment). Check your insurance eligibility.
Legacy’s at-home sperm freezing kits take the financial strain out of planning for your future. We offer several flexible options for testing and freezing your sperm, with annual, 5-year, and lifetime storage options, all at a fraction of traditional sperm freezing costs.
References
- W Ombelet et al. “Artificial insemination history: hurdles and milestones.” Facts Views Vis Obgyn, 2015.
- Keisuke Okada et al. “Recovery of Spermatogenesis Following Cancer Treatment with Cytotoxic Chemotherapy and Radiotherapy.” The World Journal of Men’s Health, 2019.
- Marion Delessard et al. “Exposure to Chemotherapy During Childhood or Adulthood and Consequences on Spermatogenesis and Male Fertility.” International Journal of Molecular Sciences, 2020.
- F. Schneider et al. “Andrology of male-to-female transsexuals: influence of cross-sex hormone therapy on testicular function.” Andrology, 2017.
- Phillp J. Cheng at el. “Fertility concerns of the transgender patient.” Translational Andrology and Urology, 2019.
- Marissa A. Kent et al. “Effects of Feminizing Hormones on Sperm Production and Malignant Changes: Microscopic Examination of Post Orchiectomy Specimens in Transwomen.” Urology, 2018.
- Peter Y. Liu et al. “Rate, extent, and modifiers of spermatogenic recovery after hormonal male contraception: an integrated analysis.” Lancet, 2006.
- Emily P. Barnard et al. “Fertility Preservation Outcomes in Adolescent and Young Adult Feminizing Transgender Patients.” Pediatrics, 2019.
- Kai Li et al. “Sperm cryopreservation of transgender individuals: trends and findings in the past decade.” Andrology, 2018.
- Abhishek P. Patel et al. “Vasectomy reversal: a clinical update.” Asian Journal of Andrology, 2016.
- Ranjith Ramasamy et al. “Vasectomy and vasectomy reversal: An update.” Indian Journal of Urology, 2011.
- Paul Claman et al. “Men at Risk: Occupation and Male Infertility.” Sexuality, Reproduction & Menopause, 2004.
- FM Shakhatreh et al. “Reproductive health of male radiographers.” Saudi Med Journal, 2001.
- FR Ochsendorf et al. “Sexually transmitted infections: impact on male fertility.” Andrologia, 2008.
- Bhavni Oberoi et al. “Study of human sperm motility post cryopreservation.” Medical Journal, Armed Forces India, 2014.
- JK Sherman et al. “Synopsis of the use of frozen human semen since 1964: state of the art of human semen banking.” Fertility & Sterility, 1973.
- RP Dickey et al. “Comparison of the sperm quality necessary for successful intrauterine insemination with World Health Organization threshold values for normal sperm.” Fertility & Sterility, 1999.
- Hamoun Rozati et al. “Process and Pitfalls of Sperm Cryopreservation.” Journal of Clinical Medicine, 2017.
- Chuan Huang et al. “Long-term cryostorage of semen in a human sperm bank does not affect clinical outcomes.” Fertility & Sterility, 2019.
- Leslee L. Subak, MD et al. “Therapeutic donor insemination: A prospective randomized trial of fresh versus frozen sperm.” American Journal of Obstetrics & Gynecology, 1992.
- Yvon Englert, MD et al. “Is fresh or frozen semen to be used in in vitro fertilization with donor sperm?” Fertility & Sterility, 1989.
- Selahittin Cayan et al. “A comparison of ICSI outcomes with fresh and cryopreserved epididymal spermatozoa from the same couples.” Human Reproduction, 2001.
- Kenan Omurtag et al. “Sperm Recovery and IVF after Testicular Sperm Extraction (TESE): Effect of Male Diagnosis and Use of Off-Site Surgical Centers on Sperm Recovery and IVF.” PLoS One, 2013.