High-quality embryos are embryos that are genetically healthy and developing properly, and are more likely to lead to a successful pregnancy. This is an important factor affecting the success of in vitro fertilization (IVF) treatment. But what constitutes embryo quality? And how does the quality of sperm impact embryo quality?
Read on to find out how embryo quality is scored, and how lifestyle factors and supplements can help increase your likelihood of success with IVF.
Key takeaways
- Embryo quality is one of the main predictors of IVF success. Sperm and egg quality both affect embryo quality.
- Embryo quality is “graded” on a number of physical and developmental metrics.
- “Aneuploidy” refers to genetic abnormalities in the embryo. Aneuploidy can be determined using preimplantation genetic testing (PGT).
- Healthy lifestyle habits and certain supplements may help improve pregnancy rates if implemented before beginning IVF.
What is embryo quality, and why is it important?
“Embryo quality” is a term used to refer to a collection of metrics concerning the development and health of the embryo. A number of factors are reflected in the embryo quality score:
- The number of cells in the embryo
- The size, structure, and appearance of the cells
- The degree of expansion the embryo has taken
Physicians rely on a complex embryo grading system to decide which embryos to transfer as well as the best day to transfer. Scoring typically begins on day three after fertilization, though grading may continue until day five as the embryo reaches blastocyst stage. Selecting only the healthiest embryos for transfer can increase the chance of success each cycle, and decrease the likelihood of miscarriage.
How embryo quality predicts fertility success
Research shows embryo quality is one of the main predictors of success in IVF cycles — in fact, embryo quality scoring predicts an embryo’s success rate even more accurately than parental age.
A 2014 study found that clinical pregnancy and live birth rates per IVF transfer were nearly two-fold higher with the transfer of a single good quality embryo than with the transfer of a poor quality embryo. Embryo quality grading, along with preimplantation genetic testing, has been the driving force behind the shift toward single embryo transfer in the fertility field over the past decade.
Embryo quality is also associated with adverse outcomes for the pregnancy. Lower quality embryos are more likely to result in miscarriage. And poor embryo quality has been shown to correlate with a significantly higher risk of low birthweight, as shown in this 2020 study out of Shanghai.
A poor embryo score doesn’t necessarily mean the embryo has no chance of success — just that it’s less likely to result in pregnancy, based on specific metrics. One study found that even poor quality embryos that made it to clinical pregnancy had a similar chance of reaching live birth, compared to a high quality embryo.
Creating an embryo: the IVF process
Only embryos created via in vitro fertilization can be graded for quality. In vitro fertilization is a fertility treatment in which an egg is combined with sperm outside of the body, in vitro, or “in glass” (in the lab). It’s a fertility treatment commonly used in cases of fallopian tube damage or absence, low ovarian reserve, or male-factor infertility.
First, the ovulatory process is stimulated using hormone medications. These drugs allow the body to generate as many mature eggs as possible, which increases the chances of a successful fertilization.
After eggs have sufficiently matured, they’re retrieved from ovaries in a brief surgical procedure and fertilized by sperm in a lab. The fertilized eggs are then allowed to develop for two to six days, during which the quality of embryos are carefully monitored and evaluated. It’s at this point that embryo quality can be scored, and preimplantation genetic testing for embryo aneuploidy can be performed.
The healthiest embryo(s) can then be transferred to a uterus to create a pregnancy. One full cycle of IVF lasts about three weeks.
How embryo quality is graded
An embryo is scored to indicate its potential for successful implantation and development. This score may change over time as the embryo is consistently evolving, and embryos may develop at different rates.
Though embryo scoring typically begins on day three after fertilization, some assessments can be made on day one, a mere 16 to 18 hours after insemination. These assessments include evaluating the pronuclear size, the size and number of nucleolar precursor bodies, and the cytoplasmic appearance. The embryo should be able to complete its first mitotic division by 27 hours after insemination.
Day 3 embryo quality scoring
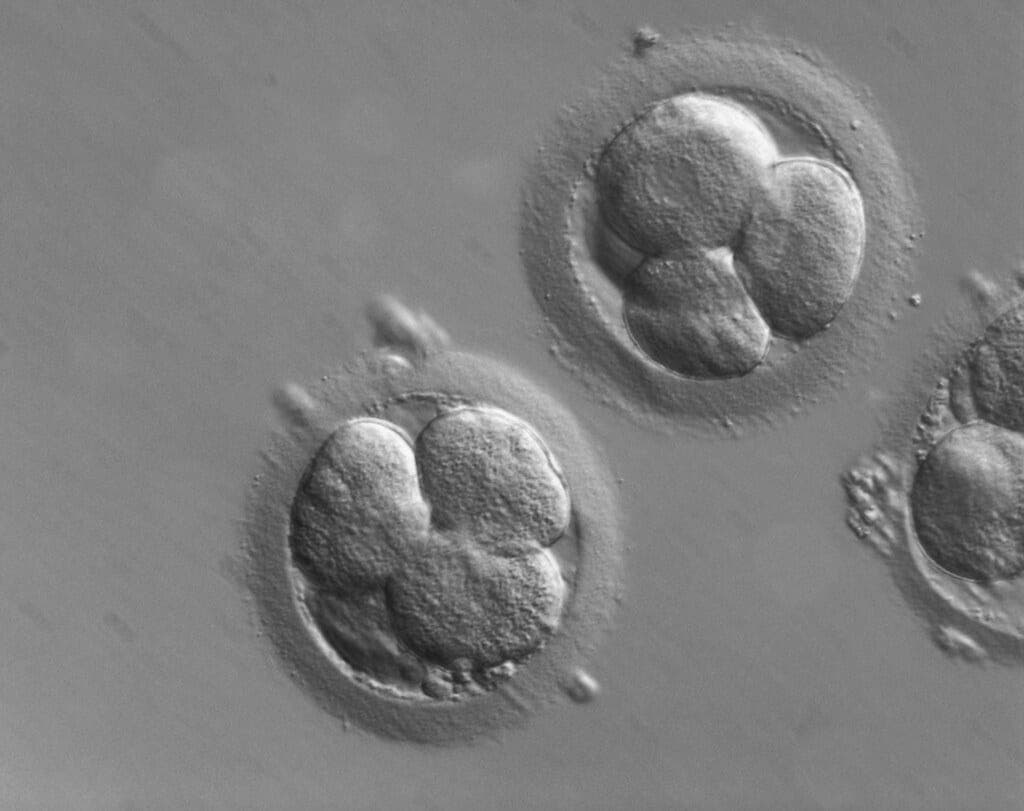
Day 3 after fertilization is called the “cleavage” stage, during which the cells inside the fertilized egg are dividing. When evaluating embryo quality on day 3, a high-powered microscope is used to assess the structure of the embryo, including the number of cells and the appearance of those cells, now called blastomeres.
Research shows that successful day 3 embryos have eight or more cells. Each of these cells should be roughly equal in size and contain a nucleus. Day 3 embryos are also checked for fragmentation, or tiny structures in the embryo detached from the cells. The embryo cells should be compacted and getting ready for the next stage of development.
Different clinics and IVF labs have different scoring systems, but day 3 embryos are typically scored 1–5, with 1 as the best score.
Day 5 embryo quality scoring
When an embryo reaches day 5, it is considered a blastocyst. At this stage, the embryo is beginning to expand and differentiate into sections and structures. Day 5 blastocysts are scored on their degree of expansion on a scale of 1–6, 6 being the most developed.
The development of the inner cell mass — the part of the embryo that becomes a fetus — is also evaluated and scored A to C, with A being the best quality. The quality of epithelium, the part of the embryo that forms the placenta and other tissues, is assessed and scored A to C, with A also indicating the best quality.
Therefore, the best day 5 embryo quality would be “6AA,” and the least optimal embryo quality score would be “1CC.”
Embryo quality vs. aneuploidy
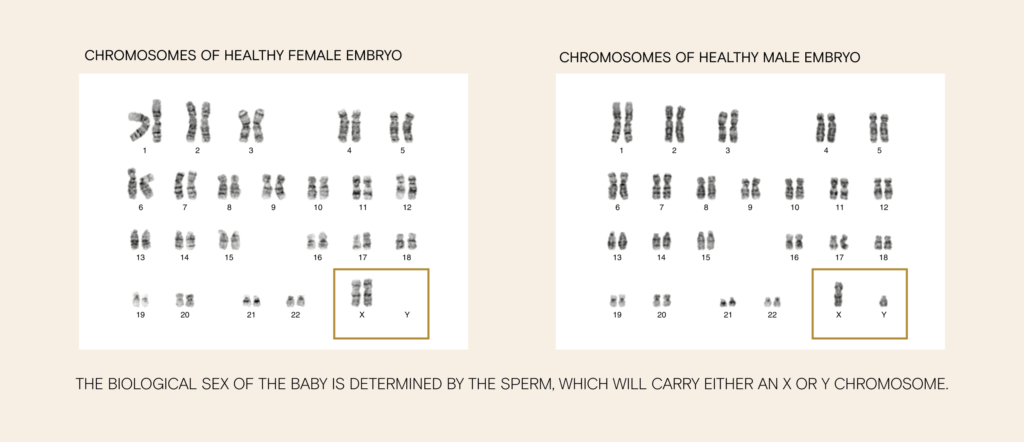
Aneuploidy refers to a genetic abnormality in which there are missing or extra chromosomes in an embryo. The correct number of chromosomes is 46 (23 pairs). Aneuploidy can result in embryos that don’t develop, resulting in infertility or IVF cycle failure, early pregnancy loss, or, more rarely, genetic disorders. The risk of creating aneuploid embryos increases with advanced parental age.
The most common aneuploidy causing genetic disorders is trisomy, in which there is an extra (so, 3 total copies) of one chromosome. Down syndrome, Patau syndrome, Klinefelter syndrome, and Edwards syndrome are all examples of trisomy disorders.
Monosomy is another kind of aneuploidy, in which there is a missing chromosome. Turner syndrome is a common monosomy, where there is a missing or damaged X chromosome.
Aneuploidy in embryos created by IVF is tested with a screening called preimplantation genetic testing (PGT-A).
While embryo quality and genetic health are separate measures, they both contribute to the success of the embryo, and they are correlated. A 2014 study of IVF patients showed that the best quality blastocysts (grade A) were majority (68%) euploid, or chromosomally normal — compared to just 20% for poor quality blastocysts.
Embryo genetic testing
Preimplantation genetic testing (PGT) is a screening test used to identify genetic defects in embryos created through in vitro fertilization. PGT-A screens for aneuploidy; PGT-M or “monogenic” screens for specific single-gene disorders, such as cystic fibrosis. Ideal candidates for this screening include patients with a history of genetic disorders, those with advanced maternal age, and individuals with a history of recurrent miscarriages or failed IVF cycles.
To perform PGT, when the embryo reaches blastocyst stage, an embryologist will take a small sample of cells (called an “embryo biopsy”) to send for genetic analysis. Embryos are typically then frozen while test results are pending.
Typically, PGD is accompanied by embryo quality grading in the process of choosing the healthiest embryos for implantation.
How sperm health affects embryo quality
Though the age of the egg (maternal age) is one of the strongest predictors of IVF success, sperm health may also influence embryo quality.
Studies show that poor semen parameters (including low sperm count and motility) are more likely to result in low blastocyst formation rates after IVF. Additionally, embryo development can also be influenced by the quality of the DNA in the sperm head. Research has found a significant correlation between sperm DNA fragmentation, or damage, and blastocyst development rates after IVF. Sperm DNA fragmentation isn’t measured in a typical semen analysis, but is typically correlated with sperm morphology and motility scores.
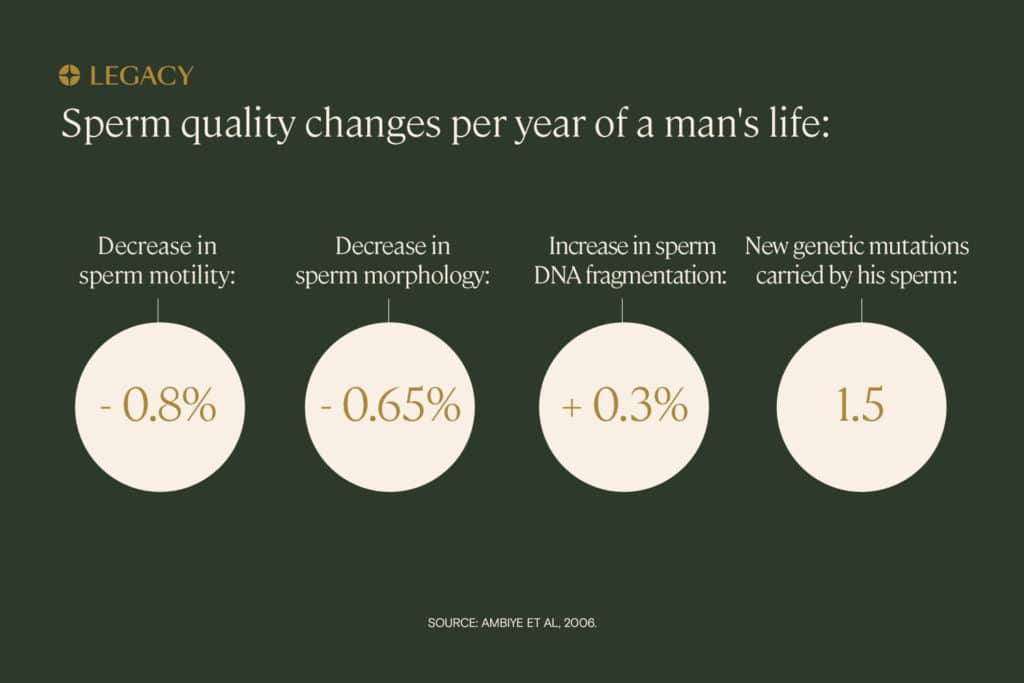
Sperm health decreases with age. That’s likely why research has shown that advanced paternal age (40+) is associated with a decreased number of IVF embryos that reached blastocyst stage, as well as an increased risk of embryo aneuploidy.
Improve sperm health before IVF
You can make lifestyle choices that may improve sperm health before starting the IVF process. This includes following a healthy diet, exercising regularly, and taking certain male fertility supplements. If you’ve experienced poor embryo quality after an IVF cycle, you may want to talk to your doctor and implement some changes to support sperm health.
Lifestyle choices to improve sperm quality
In a 2020 study of pre-conceptual care for couples seeking fertility treatment, physical exercise in men was shown to improve semen parameters and reduce seminal markers of inflammation and oxidative stress, leading to increased pregnancy rates. Other lifestyle factors that may positively influence sperm health before IVF include cutting back on smoking, alcohol, and caffeine.
Learn more about how to improve male fertility.
Supplements
Taking specific, evidence-based male fertility supplements may also help improve sperm health. For instance, CoQ10 is an antioxidant shown to improve sperm concentration, motility, and morphology. Studies show that taking L-carnitine for several weeks prior to IVF with ICSI was shown to improve sperm quality and increase fertilization rates by 11.5%.
Explore other male fertility supplements and medication for male fertility.
The best starting point in the IVF journey is understanding the quality of your sperm right now. Try an at-home semen analysis kit or at-home sperm DNA fragmentation analysis.